The human body’s metabolic machinery relies on a tightly regulated system of hormonal signals, none more critical than insulin. As a central player in glucose regulation, insulin orchestrates the uptake and storage of sugar across various tissues. However, when this system malfunctions—either through disease, medical error, or inappropriate therapeutic intervention—the results can be catastrophic. One of the most severe consequences is an insulin coma, a life-threatening condition that demands immediate attention and precise management. Although relatively rare in modern clinical practice, the implications of insulin coma span across endocrinology, pharmacology, and emergency medicine, making it a condition of both clinical urgency and academic intrigue.
You may also like: How Diabetes Affects the Brain: Understanding Brain Fog, Memory Loss, and Mental Confusion from High Blood Sugar
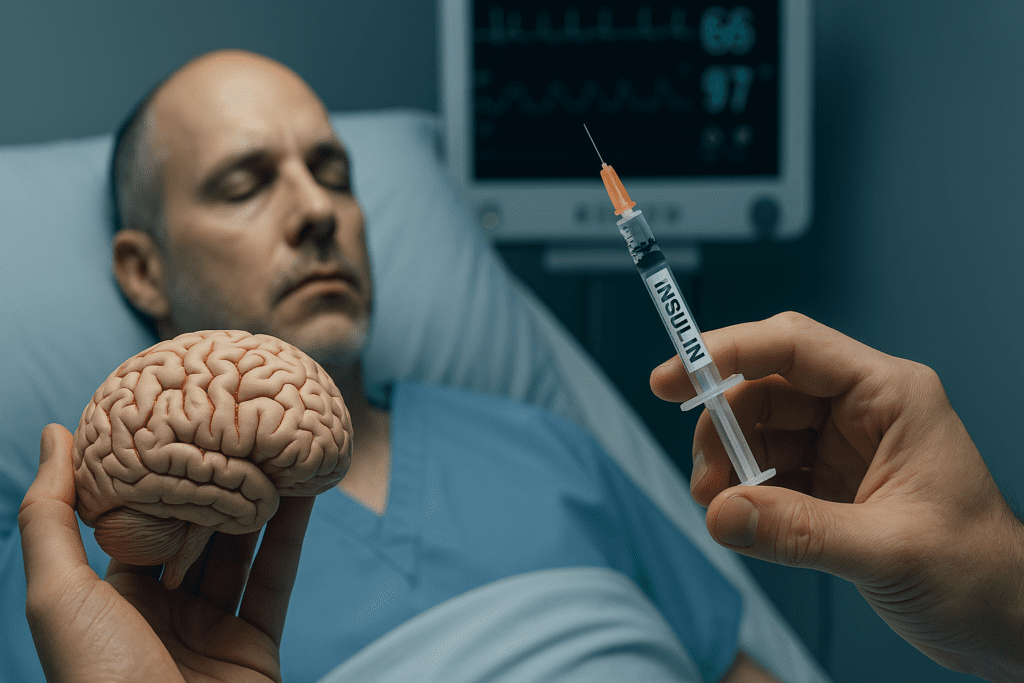
An insulin coma is not merely a side effect of excessive insulin but rather the endpoint of a complex physiological cascade. It typically arises when insulin levels dramatically exceed the body’s current glucose availability, driving blood sugar to dangerously low levels. When cerebral glucose supply is critically impaired, consciousness falters—first subtly, then catastrophically. The ensuing state is not just unconsciousness; it is a metabolic crisis. Understanding insulin coma through the lens of contemporary science requires more than a superficial grasp of diabetes or hypoglycemia. It involves dissecting hormonal dynamics, recognizing patient-specific vulnerabilities, and appreciating the nuanced approaches to insulin coma treatment that modern medicine has developed.
This article explores the causes, clinical risks, diagnostic intricacies, and emerging treatment strategies associated with insulin coma. It bridges scientific evidence with practical applications to offer a comprehensive resource for healthcare professionals, medical students, and curious minds seeking to understand one of the most severe manifestations of insulin-related dysfunction.
Defining Insulin Coma and Its Underlying Mechanisms
To understand insulin coma at its core, one must first appreciate the foundational physiology of glucose and insulin balance. Under normal conditions, insulin facilitates the transport of glucose from the bloodstream into cells, particularly muscle and fat tissue. This action helps maintain blood glucose levels within a narrow, optimal range. When insulin is present in appropriate amounts, it supports cellular function, energy metabolism, and overall homeostasis. However, when insulin levels become excessive—whether from endogenous overproduction, exogenous administration, or pharmacologic miscalculation—the balance is disrupted.
An insulin coma occurs when hypoglycemia becomes so profound that neuronal activity is suppressed, leading to loss of consciousness. The brain, unlike other tissues, depends almost exclusively on glucose for its energy supply. Therefore, when glucose levels drop precipitously, the brain’s ability to function is swiftly compromised. Symptoms may begin with confusion, blurred vision, and agitation. If not promptly addressed, these can escalate to seizures, unconsciousness, and eventually, coma. The clinical progression is rapid and unforgiving, often occurring within minutes to hours depending on the severity of hypoglycemia.
Endocrinologically, this condition reflects not only a glucose deficit but also a cascade of hormonal imbalances. Counter-regulatory hormones such as glucagon, cortisol, and adrenaline attempt to correct hypoglycemia, but their efforts can be outmatched by overwhelming insulin activity. This hormonal tug-of-war underscores the complexity of insulin coma and explains why its treatment must go beyond simple glucose replacement.
Common Triggers and Risk Factors Associated with Insulin Coma
Insulin coma is not always the result of accidental overdose or medical error; it can also stem from complex physiological interactions or even deliberate actions. In individuals with diabetes—particularly those with type 1 diabetes—exogenous insulin therapy is a cornerstone of management. However, incorrect dosing, erratic meal patterns, excessive exercise without proper adjustments, or delayed absorption of insulin can precipitate dangerously low blood sugar levels. The vulnerability is compounded by factors such as renal insufficiency, which impairs insulin clearance and can prolong its effects in the body.
Another risk group includes individuals with insulinomas—rare pancreatic tumors that secrete excessive insulin independently of blood glucose levels. These tumors can be insidious, causing unpredictable episodes of hypoglycemia that may culminate in insulin coma if undiagnosed or untreated. Additionally, autoimmune conditions such as insulin autoimmune syndrome (Hirata’s disease) can result in fluctuating insulin levels that confuse both patient and clinician alike.
Intentional misuse of insulin, seen in cases of Munchausen syndrome or attempted suicide, also contributes to the incidence of insulin coma. These scenarios are especially complex because they may involve large quantities of long-acting insulin formulations, making recovery more difficult and treatment timelines less predictable. Elderly patients, those with cognitive impairments, or individuals with limited access to proper diabetes education also face increased risk due to mismanagement or misunderstanding of insulin regimens.
The Pathophysiological Progression of Hypoglycemia to Coma
The evolution from hypoglycemia to coma follows a predictable yet perilous trajectory. In the early stages, glucose deprivation triggers a neuroglycopenic response—dizziness, confusion, weakness, and cognitive delay. These symptoms reflect the brain’s struggle to maintain function in the absence of its primary fuel. As glucose levels continue to fall, autonomic symptoms emerge: sweating, palpitations, anxiety, and tremors. These are driven by surges in adrenaline and cortisol, signaling the body’s desperate attempt to counterbalance the insulin excess.
However, when hypoglycemia becomes severe and prolonged, the brain begins to shut down higher-order functions. Speech slurs, coordination is lost, and seizures may occur due to cortical and subcortical dysfunction. At the lowest thresholds of blood sugar—typically below 30 mg/dL—consciousness is lost, marking the transition into an insulin coma. At this point, metabolic failure predominates. Neurons begin to depolarize improperly, calcium floods cells, and oxidative stress increases. If glucose is not restored rapidly, neuronal death can ensue, particularly in vulnerable brain regions such as the hippocampus and cerebral cortex.
The pathophysiology of insulin coma is not just about the lack of glucose but also the duration and depth of hypoglycemia. Short episodes can be reversed with minimal long-term impact, but prolonged comas may result in permanent cognitive deficits, motor impairments, or even death. Understanding this timeline is essential for early recognition and timely intervention.
Diagnostic Challenges in Identifying Insulin Coma
Diagnosing an insulin coma presents a unique set of challenges, especially in emergency or pre-hospital settings. The symptoms can mimic other neurologic events such as strokes, seizures, or drug intoxication. Without immediate access to a glucometer or laboratory facilities, first responders may find it difficult to distinguish insulin coma from other causes of unconsciousness.
The Whipple’s triad remains a cornerstone for diagnosis: symptoms of hypoglycemia, low plasma glucose at the time of symptoms, and resolution of symptoms after glucose administration. However, in a comatose patient, this triad cannot always be fully assessed. Rapid point-of-care glucose testing becomes vital in such scenarios. If blood sugar is found to be severely low and the clinical history includes insulin use or diabetes, the presumptive diagnosis of insulin coma can be made with reasonable confidence.
Further diagnostic steps may involve assessing insulin and C-peptide levels, particularly if an insulinoma is suspected or if intentional overdose is a possibility. Toxicology screens, imaging studies, and endocrine panels may be required to rule out alternative explanations or complicating factors. The diagnostic journey often continues even after initial stabilization, as the underlying cause must be addressed to prevent recurrence.

Immediate and Long-Term Insulin Coma Treatment Strategies
Treating insulin coma is a time-sensitive and multifaceted process. The cornerstone of immediate management is the rapid restoration of plasma glucose. In conscious patients who can swallow, oral glucose or sugary drinks may suffice. In comatose individuals, intravenous dextrose—usually in the form of 50% dextrose (D50)—is the treatment of choice. Intramuscular glucagon may also be administered, especially in out-of-hospital settings or when IV access is unavailable.
However, insulin coma treatment does not end with glucose correction. Continuous monitoring is essential to ensure that glucose levels stabilize without swinging into hyperglycemia, which can create additional complications. In cases involving long-acting insulin overdoses or insulinomas, glucose infusions may need to be continued for many hours, if not days. Electrolyte imbalances, particularly hypokalemia, must also be corrected during the refeeding phase.
Long-term treatment focuses on identifying and addressing the root cause of the insulin coma. For patients with diabetes, this may involve reassessing insulin regimens, providing diabetes education, and introducing continuous glucose monitors (CGMs) for real-time feedback. In cases involving insulin-secreting tumors, surgical resection is often necessary. Psychological evaluation may be required in instances of intentional overdose to prevent recurrence. By combining acute intervention with long-term management, healthcare providers can reduce the likelihood of future episodes and mitigate potential neurologic damage.
Neurocognitive and Systemic Consequences of Insulin Coma
The aftermath of insulin coma can extend far beyond the acute episode. Depending on the severity and duration of hypoglycemia, patients may experience lingering cognitive impairments such as memory loss, difficulty concentrating, or reduced executive function. These effects are particularly concerning in children and older adults, whose brains may be more vulnerable to glucose deprivation.
Research has shown that even brief episodes of profound hypoglycemia can produce lasting changes in brain metabolism and structure. Functional MRI studies reveal altered connectivity in key networks, and animal models suggest a role for oxidative stress and inflammation in mediating long-term damage. These insights highlight the need for proactive cognitive screening and rehabilitation following insulin coma.
Systemically, repeated or prolonged hypoglycemia has been associated with cardiovascular events, including arrhythmias and sudden cardiac death. The autonomic stress response, while protective in the short term, can have deleterious effects on the heart, especially in those with preexisting cardiovascular disease. This underscores the importance of comprehensive care that goes beyond glucose correction to include cardiovascular monitoring and support.
Evolving Tools in Prevention and Monitoring
The future of insulin coma prevention lies in technology and education. Continuous glucose monitors (CGMs) and insulin pumps with predictive algorithms now offer real-time alerts and automated insulin adjustments. These tools significantly reduce the risk of severe hypoglycemia by alerting users—and in some cases, automatically suspending insulin delivery—before glucose levels become dangerously low.
Artificial pancreas systems, which combine CGMs with closed-loop insulin delivery, represent the next frontier in diabetes management. Early trials have shown promising reductions in both hyper- and hypoglycemic episodes. Education remains equally vital. Patients must understand not only how to dose insulin but how to adjust for variables such as stress, illness, physical activity, and meal composition.
Clinical practice guidelines increasingly emphasize individualized care plans, integrating lifestyle factors, patient preferences, and comorbidities into insulin management strategies. By combining technological advancements with personalized care, the incidence of insulin coma can be further reduced, enhancing both safety and quality of life for insulin users.
The Role of Public Health and Policy in Reducing Insulin-Related Harm
While medical professionals play a crucial role in preventing and managing insulin coma, public health initiatives and policy reforms are equally important. Access to affordable insulin, education on diabetes management, and widespread availability of emergency glucose administration tools like glucagon kits can make the difference between life and death.
Policy reforms aimed at regulating insulin pricing and improving healthcare access are especially relevant in low-income and underinsured populations, where diabetes-related complications—including insulin coma—are more prevalent. Schools, workplaces, and public venues should be equipped with basic knowledge and tools to respond to diabetic emergencies. Encouraging community awareness can reduce stigma and promote quicker intervention during hypoglycemic events.
Training healthcare professionals to recognize subtle signs of hypoglycemia and to counsel patients effectively about risk reduction is another key strategy. When coupled with systemic changes in healthcare delivery and community engagement, these efforts can create a safer environment for individuals at risk of insulin coma.
Looking Ahead: Research Directions and Knowledge Gaps
Despite advances in technology and clinical practice, significant gaps remain in our understanding of insulin coma. Future research must explore the neurobiology of hypoglycemia-induced coma, including the cellular mechanisms behind neuronal injury and recovery. Understanding why certain individuals suffer permanent damage while others recover fully could inform personalized treatment protocols.
There is also a need to investigate gender, age, and genetic variations in response to hypoglycemia. Such studies could illuminate why some populations are more susceptible to insulin-related complications. Additionally, the role of gut microbiota, circadian rhythms, and micronutrient status in modulating insulin sensitivity and glucose metabolism is gaining attention and could yield insights relevant to both prevention and recovery from insulin coma.
Emerging pharmacologic agents that modulate insulin action or enhance endogenous glucose production may offer new avenues for intervention. As the scientific community continues to unravel the complexities of insulin biology, the ultimate goal remains clear: to prevent insulin coma through better understanding, better tools, and better care.
Frequently Asked Questions (FAQ): Exploring the Deeper Dimensions of Insulin Coma and Its Treatment
1. How did insulin coma historically influence psychiatric treatment innovation?
The history of insulin coma represents a pivotal moment in the evolution of psychiatric care. While it’s no longer used, the therapy laid the foundation for experimental biological treatments in psychiatry. Before antipsychotics were developed, insulin coma treatment reflected a bold, if controversial, approach to managing schizophrenia and severe mental illness. The treatment’s intensive monitoring protocols pushed the medical community to adopt more comprehensive psychiatric nursing care. Though outdated, insulin coma experiments indirectly advanced ethical standards and ushered in more rigorous frameworks for patient safety and consent in medical research.
2. What are the long-term neurological effects associated with repeated insulin comas?
Patients subjected to repeated insulin coma episodes historically faced potential neurological consequences, some of which are still being studied through retrospective analysis. Emerging research suggests that recurrent hypoglycemia induced by insulin coma treatment may have subtly impaired cognitive resilience in certain individuals. While structural brain damage was rare, deficits in memory consolidation and attention have been reported in long-term follow-up studies. Additionally, some patients experienced persistent mood dysregulation that may have been linked to repeated metabolic stress. These findings are important for understanding how extreme interventions can influence brain function beyond their immediate therapeutic goals.
3. Are there any parallels between insulin coma treatment and modern therapeutic hypothermia?
Surprisingly, there are conceptual overlaps between insulin coma and modern therapeutic hypothermia, especially in terms of controlled systemic shutdown to promote neurological reset. While the mechanisms differ—glucose deprivation versus temperature modulation—both approaches aim to influence brain chemistry under tightly supervised conditions. Modern hypothermia, used post-cardiac arrest or in neonatal encephalopathy, requires the same level of intensive monitoring once demanded by insulin coma treatment. These parallels underscore the continued medical fascination with using physiological extremes to trigger therapeutic outcomes, albeit with far greater safety and scientific backing today.
4. Can metabolic research from the insulin coma era inform current diabetes care?
Yes, surprisingly, some of the foundational observations from insulin coma experiments have informed modern endocrinology, particularly in the understanding of hypoglycemia’s systemic effects. While insulin coma treatment is no longer ethically acceptable, it provided early clinical insights into glucose-regulation thresholds, organ responses, and autonomic dysfunction during glucose deprivation. These insights helped refine modern glucose-monitoring protocols and emergency response strategies for diabetic patients at risk of severe hypoglycemia. In this way, historical misuse has indirectly contributed to life-saving interventions in current diabetes management.
5. How does insulin coma treatment reflect the evolution of medical ethics?
Insulin coma marked a significant turning point in how the medical community began evaluating the ethical implications of aggressive therapies. Initially administered without full patient consent, the treatment highlighted glaring gaps in ethical oversight. As adverse events accumulated, insulin coma prompted calls for stricter institutional review boards and informed consent procedures. Modern bioethics owes much of its foundational momentum to the scrutiny and eventual abandonment of treatments like insulin coma. Today’s clinical research standards—especially in psychiatry—are a direct response to this historical experience.
6. Could insulin coma ever make a return in any modified, evidence-based form?
While a return to full-scale insulin coma treatment is highly unlikely due to safety concerns, some researchers have speculated on its metabolic principles being repurposed. For instance, targeted insulin modulation—not coma induction—is being explored for its effects on neuroinflammation and neurotransmitter regulation. There’s also interest in using tightly controlled hypoglycemia in animal models to better understand neuronal recovery mechanisms. Any such revival would bear no resemblance to the original insulin coma but may involve microdosing strategies or glucose-oscillation therapies in neurologically monitored settings. These future possibilities show that even discarded treatments can inspire valuable innovation when revisited responsibly.
7. What psychological impact did insulin coma therapy have on patients post-recovery?
Beyond physical risks, many patients reported long-lasting psychological effects following insulin coma. Some described a lingering sense of vulnerability or existential confusion, possibly stemming from repeated near-death experiences. Even in cases where behavioral improvements were noted, the trauma of the experience often left psychological scars. The treatment environment—often involving restraint and loss of bodily autonomy—contributed to feelings of helplessness and mistrust in medical professionals. These aftereffects have become critical case studies in patient-centered psychiatric care, shaping how modern interventions are designed to minimize psychological harm.
8. How did insulin coma treatment influence hospital infrastructure and interdisciplinary care?
Managing insulin coma demanded constant coordination between psychiatrists, endocrinologists, nurses, and dietitians, inadvertently fostering the modern model of interdisciplinary care. Hospitals were required to install special observation units, maintain high-calorie recovery foods, and provide real-time glucose monitoring—an infrastructure not common in psychiatric settings at the time. This level of complexity highlighted the need for integrated care models, especially for medically fragile psychiatric patients. In many ways, the operational demands of insulin coma treatment catalyzed advancements in medical-psychiatric liaison services, a practice that is now standard in hospitals worldwide.
9. What lessons can be learned from insulin coma in the context of experimental treatments today?
One of the key takeaways from insulin coma treatment is the importance of balancing innovation with patient safety. Many experimental treatments carry initial enthusiasm before long-term outcomes are understood, and insulin coma serves as a historical reminder of this risk. Today’s ethical trials in psychedelic therapy and neuromodulation benefit from protocols developed in the wake of insulin coma’s scrutiny. Patient-centered metrics, ethical committees, and real-time adverse event tracking are now considered essential, precisely because of missteps in earlier treatment eras. Learning from insulin coma ensures that the same mistakes are not repeated under new medical guises.
10. Are there modern technologies that could have made insulin coma treatment safer if they existed at the time?
If technologies like continuous glucose monitors (CGMs), AI-based risk prediction, and real-time telemetry had existed during the era of insulin coma, the treatment could have been vastly safer—though still ethically questionable. Real-time monitoring might have prevented many of the adverse events historically associated with insulin coma treatment. Machine learning algorithms could have predicted which patients were at higher risk for complications or poor responsiveness. These tools also allow clinicians to simulate outcomes, which would likely have dissuaded widespread adoption of such a high-risk therapy in the first place. Even so, the inherent dangers of insulin coma underscore that technology alone cannot justify ethically flawed practices.

Conclusion: Advancing Awareness and Solutions for Insulin Coma Through Scientific Insight
Insulin coma represents one of the most extreme consequences of glucose regulation gone awry. It is a sobering reminder of the delicate balance that underlies human metabolism and the importance of vigilant, informed insulin management. By dissecting its causes, recognizing its warning signs, and embracing both old and new strategies for insulin coma treatment, the medical community can turn this potentially fatal condition into a preventable one.
Scientific insight continues to evolve, offering deeper understanding into the physiologic disruptions that lead to insulin coma and the neurologic damage it can cause. With advances in glucose monitoring, insulin delivery systems, and personalized treatment approaches, the future holds promise for reducing the incidence and severity of insulin-related emergencies.
Ultimately, public awareness, clinical vigilance, and continued research form the triad that can reshape how we approach insulin coma—not just as a medical crisis, but as an opportunity for innovation and improved patient care. The journey from crisis to comprehension is one paved with science, compassion, and the unrelenting pursuit of better outcomes.
glucose regulation and brain function, hypoglycemia symptoms, insulin overdose complications, diabetes emergency response, long-acting insulin risks, blood sugar monitoring technology, insulin pump safety, continuous glucose monitoring devices, endocrinology research insights, neurobiology of hypoglycemia, glucose repletion therapy, glucagon rescue kits, metabolic crisis treatment, cognitive recovery after coma, insulin therapy side effects, hormonal imbalance and coma, insulinoma diagnosis, diabetes education programs, cardiovascular impact of hypoglycemia, artificial pancreas systems
Further Reading:
Role of Insulin in Health and Disease: An Update
Trends in insulin resistance: insights into mechanisms and therapeutic strategy
Disclaimer: The content published on Better Nutrition News (https://betternutritionnews.com) is for informational and educational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified healthcare professional before making any changes to your diet, nutrition, or wellness practices. The opinions expressed by authors and contributors are their own and do not necessarily reflect those of Better Nutrition News.
Better Nutrition News and its affiliates make no representations or warranties regarding the accuracy, completeness, or reliability of the information provided. We disclaim all liability for any loss, injury, or damage resulting from the use or reliance on the content published on this site. External links are provided for reference purposes only and do not imply endorsement.



