Introduction
The colon, a vital part of the digestive system, plays an essential role in absorbing water and nutrients while preparing waste for elimination. Despite being integral to overall digestive health, colon-related issues often go unnoticed until they become severe. This oversight can be due to vague or overlapping symptoms, misattribution to temporary digestive discomfort, or even the stigma surrounding gastrointestinal conversations. Yet, recognizing colon issues symptoms early can be the difference between a manageable condition and a life-altering diagnosis.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
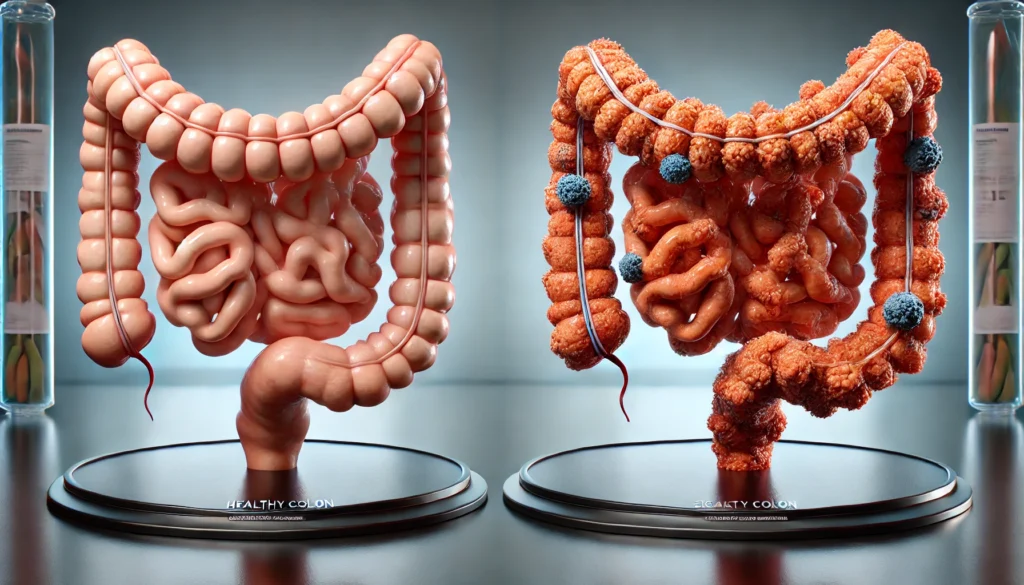
Colon problems can manifest in various ways, including changes in bowel habits, abdominal discomfort, bloating, and unexplained weight loss. While these symptoms can occasionally be benign, they may also point to more serious underlying colon problems such as diverticulitis, ulcerative colitis, irritable bowel syndrome (IBS), colorectal polyps, or even colon cancer. Understanding the early colon problem symptoms empowers individuals to seek timely medical intervention and make informed decisions about their health.
This comprehensive article delves deep into the physiology of the colon, the root causes of dysfunction, diagnostic pathways, and evidence-based treatment strategies. It highlights how colon issues symptoms can vary in intensity and duration and emphasizes the importance of distinguishing between functional and structural problems. In alignment with EEAT (Experience, Expertise, Authoritativeness, and Trustworthiness) principles, the content is rooted in current clinical research and medical consensus, offering readers both clarity and confidence. Whether you are concerned about persistent digestive symptoms or simply want to educate yourself on colon health, this guide offers an in-depth, medically accurate resource built on science and empathy.

Anatomy and Function of the Colon: Why It Matters
To fully appreciate the implications of colon problems, it’s important to understand what the colon does and why it’s so vital. The colon, or large intestine, is the final segment of the gastrointestinal tract. It extends from the cecum (connected to the small intestine) to the rectum and anus. Its primary function is to absorb water and electrolytes from undigested food, form stool, and facilitate its passage out of the body.
Beyond its mechanical roles, the colon houses trillions of bacteria collectively known as the gut microbiota. These microorganisms assist in fermentation of indigestible carbohydrates, production of certain vitamins (like K and B12), and immune system modulation. When the colon’s environment is disrupted—whether by inflammation, infection, or obstruction—the result is often reflected in noticeable colon issues symptoms. Disruption of the mucosal lining, abnormal motility, or overgrowth of harmful bacteria can cause significant discomfort and systemic consequences.
Colon problems are not only painful or inconvenient—they are often indicators of deeper physiological imbalances. Whether the issue lies in the structural integrity of the colon walls or in its functional coordination with the rest of the digestive system, understanding how the colon works is crucial for interpreting colon problem symptoms and addressing them effectively.

Common Colon Issues Symptoms: What to Watch For
Colon issues symptoms can be subtle at first, gradually intensifying over time. They are often mistaken for everyday digestive troubles, which delays diagnosis and treatment. However, certain signs warrant close attention, especially when persistent.
A frequent symptom associated with colon problems is a change in bowel habits. This can mean constipation, diarrhea, or fluctuations between the two. Irregular bowel movements may be a response to functional issues like IBS or signal more serious concerns such as partial obstruction or inflammatory bowel disease (IBD).
Another common indicator is abdominal pain or cramping, often localized to the lower abdomen. This discomfort may increase after meals or be accompanied by bloating and gas. While these can be normal postprandial sensations, their chronic presence often signifies underlying colon problem symptoms that need evaluation.
Blood in the stool is a red flag symptom. While it can sometimes result from benign causes like hemorrhoids, it may also indicate colorectal polyps, diverticulosis, or colorectal cancer. Unexplained weight loss, fatigue, and anemia are systemic signs that can accompany serious colon conditions and should prompt immediate investigation.
Patients should also be mindful of sensations like incomplete evacuation, rectal pressure, or mucus in the stool, all of which are classic colon issues symptoms linked to disorders like ulcerative colitis or rectal inflammation. When these symptoms co-occur, their clinical significance becomes even greater, necessitating comprehensive diagnostic workup.
Major Causes of Colon Problems: Inflammatory, Functional, and Structural
Colon problems arise from a wide range of causes that can generally be categorized into inflammatory, functional, or structural. Each of these has distinct characteristics but often shares overlapping symptoms, making diagnosis both nuanced and essential.
Inflammatory causes include conditions like ulcerative colitis and Crohn’s disease. These are autoimmune disorders in which the immune system attacks the lining of the colon, resulting in chronic inflammation, ulceration, and tissue damage. Colon issues symptoms in these cases typically include bloody diarrhea, abdominal pain, and fatigue. The damage from chronic inflammation may also increase the risk of colorectal cancer over time.
Functional colon problems, such as irritable bowel syndrome (IBS), are characterized by abnormal muscle contractions and heightened sensitivity in the colon without visible inflammation or damage. Though less structurally damaging, IBS can cause significant distress, leading to bloating, gas, irregular bowel movements, and cramping. The symptoms often vary in severity and are influenced by stress, diet, and hormonal changes.
Structural issues include diverticulosis (pouch-like structures in the colon), colorectal polyps, and strictures (narrowing of the colon). These anatomical abnormalities may not cause symptoms immediately but can lead to serious complications such as infection (diverticulitis), obstruction, or even cancer. Colon problem symptoms from structural issues tend to be more persistent and less responsive to dietary changes alone.
Understanding which of these categories your symptoms fall into can help guide appropriate treatment strategies, ranging from anti-inflammatory medications to surgical interventions or lifestyle changes.
Colon Cancer and Polyps: When Symptoms Signal Something Serious
One of the most concerning colon problems is colorectal cancer, which often starts silently with the growth of polyps—benign lesions that can become malignant over time. The transformation from polyp to cancer is typically slow, which means early detection through screening can dramatically improve outcomes.
Colon cancer symptoms may include persistent abdominal pain, blood in the stool, changes in bowel habits, and unintentional weight loss. However, many early-stage cases present without any colon issues symptoms at all, which is why routine screening colonoscopies after age 45 (or earlier for those with a family history) are critically important.
Polyps themselves may not cause immediate colon problem symptoms but are typically discovered during colonoscopy. Removing them during the procedure can prevent progression to cancer. There are several types of polyps, including adenomatous (pre-cancerous), hyperplastic (generally benign), and inflammatory. The size, number, and histological type of polyps determine the follow-up interval for subsequent screenings.
In some cases, colon problems that appear minor—such as minor bleeding or a slight change in stool shape—may be the only early indicators of a deeper malignancy. Therefore, recognizing colon issues symptoms and seeking timely evaluation is not just about comfort, but about saving lives.
Diagnostic Tests for Colon Problems: How Doctors Identify the Cause
Diagnosing colon problems involves a thorough assessment combining symptom history, physical examination, and diagnostic testing. Physicians usually start by gathering detailed information about bowel habits, pain patterns, dietary influences, and family history. This helps narrow down potential causes of colon problem symptoms.
A physical examination may include palpation of the abdomen and a digital rectal exam. Laboratory tests such as complete blood count (CBC) can reveal signs of anemia, which may indicate chronic blood loss, while inflammatory markers like CRP (C-reactive protein) or fecal calprotectin can help detect inflammation.
Colonoscopy is the gold standard for evaluating colon issues symptoms, offering both visualization and the ability to biopsy tissue or remove polyps. Sigmoidoscopy, which examines the lower part of the colon, may be used for more focused evaluations. Imaging techniques like CT colonography and abdominal ultrasound can identify structural abnormalities such as diverticula or masses.
For functional disorders like IBS, diagnosis often relies on exclusion—ruling out organic disease—along with fulfilling the Rome IV criteria, which categorize functional GI disorders based on symptom duration and frequency.
Stool tests can identify infections, blood, or markers of inflammation. In cases where symptoms are severe or inconclusive, motility studies, capsule endoscopy, or genetic testing may be warranted. Accurate diagnosis is critical for directing effective treatment and preventing complications.

Treatment Strategies for Managing Colon Problems
Treatment for colon problems is highly individualized and depends on the underlying cause, severity of symptoms, and overall patient health. Approaches often involve a combination of pharmacologic therapy, dietary modifications, and lifestyle interventions.
Inflammatory conditions like ulcerative colitis and Crohn’s disease are treated with medications such as corticosteroids, immunomodulators, and biologic therapies that target specific immune pathways. These aim to induce remission, reduce inflammation, and prevent long-term damage. Surgical resection of the affected colon segment may be necessary in severe cases.
For functional colon problems like IBS, symptom management is the primary focus. This may include antispasmodic medications, probiotics, low-dose antidepressants, and dietary plans such as the low-FODMAP diet, which restricts fermentable sugars known to trigger symptoms. Mind-body therapies such as cognitive-behavioral therapy and stress reduction can also alleviate symptom severity.
Constipation-dominant colon issues are often addressed with increased dietary fiber, osmotic or stimulant laxatives, and hydration. Diarrhea-predominant conditions may be treated with anti-diarrheal agents, bile acid binders, or microbiome-targeted therapies.
Polyps detected during colonoscopy are typically removed to reduce the risk of malignancy. Surveillance colonoscopies are scheduled based on polyp type and risk factors. Colon cancer treatment may involve surgery, chemotherapy, radiation, or targeted biological therapies, depending on stage and molecular characteristics.
Supportive care—including nutrition counseling, psychological support, and routine follow-up—plays a crucial role in long-term management of colon problems. An integrative approach that addresses physical, emotional, and environmental contributors yields the best outcomes.
Frequently Asked Questions
1. What are the early colon issues symptoms that people should never ignore?
Early colon issues symptoms include persistent changes in bowel habits such as diarrhea, constipation, or alternating patterns, as well as abdominal pain, bloating, and blood in the stool. These symptoms, especially when chronic, may indicate underlying colon problems such as inflammatory bowel disease, polyps, or even colorectal cancer. Unexplained fatigue, anemia, or sudden weight loss should also prompt immediate medical attention, as they may signal systemic involvement.
2. How are colon problem symptoms different from general digestive discomfort?
General digestive discomfort often resolves quickly and is linked to specific triggers like diet or temporary stress. In contrast, colon problem symptoms are usually persistent, recurrent, and not easily explained by minor lifestyle changes. They often involve more specific bowel pattern changes, blood in the stool, or systemic symptoms like weight loss and fatigue. The chronic nature and intensity of colon problems typically distinguish them from benign digestive upsets.
3. Can colon problems exist without pain?
Yes, some colon problems may develop silently without causing noticeable pain, particularly in the early stages. Polyps and even colon cancer may grow asymptomatically for years. Functional disorders like constipation or diarrhea can occur without pain, though they often involve other discomforts. This is why screening and paying attention to subtle changes in bowel habits are critical, even in the absence of pain.
4. What dietary factors worsen colon issues symptoms?
Diets low in fiber and high in processed foods, sugar, and saturated fats can worsen colon problems by slowing motility, encouraging harmful microbial growth, and promoting inflammation. For individuals with IBS or inflammatory bowel conditions, specific foods like dairy, gluten, caffeine, alcohol, and fermentable carbohydrates (FODMAPs) may exacerbate colon issues symptoms. Personalized dietary interventions, guided by a dietitian, are often most effective.
5. Are all colon polyps dangerous?
Not all colon polyps are dangerous, but some types carry a higher risk of developing into cancer. Adenomatous polyps are considered pre-cancerous and require removal, while hyperplastic polyps are generally benign. Size, number, and histological features determine the level of concern. Routine colonoscopy helps identify and remove polyps early, significantly reducing the risk of colorectal cancer.
6. How do stress and mental health affect colon problems?
Stress and mental health play a significant role in functional colon problems due to the gut-brain axis. Chronic stress can alter motility, increase intestinal sensitivity, and disrupt the gut microbiota, intensifying colon issues symptoms. Conditions like IBS are particularly sensitive to psychological factors. Addressing stress through therapy, relaxation techniques, and lifestyle changes can greatly improve symptom control.
7. What are the risks of untreated colon problems?
Untreated colon problems can lead to severe complications. Inflammatory conditions may result in scarring, strictures, or even perforation. Polyps can progress to cancer if not removed. Chronic constipation can lead to fecal impaction, hemorrhoids, or rectal prolapse. Ignoring colon issues symptoms not only affects quality of life but can result in life-threatening consequences if the underlying cause is serious.
8. How often should colon cancer screenings be done?
For average-risk individuals, colonoscopy is recommended every 10 years starting at age 45. Those with a family history of colon cancer or polyps may need earlier and more frequent screening. If polyps are found, surveillance intervals depend on their type and number. Other screening options include fecal immunochemical tests (FIT) annually or stool DNA tests every 3 years. Consultation with a healthcare provider helps tailor the best approach.
9. Can children experience colon problems?
Yes, children can experience colon problems, though they often differ from adult conditions. Functional constipation is common in children, often due to diet or behavioral patterns. Inflammatory bowel diseases can also present during adolescence. Symptoms like abdominal pain, bloody stools, and weight loss in children should never be ignored. Pediatric evaluation and specialized care are essential for proper diagnosis and treatment.
10. What lifestyle changes support long-term colon health?
Key lifestyle changes that support colon health include eating a fiber-rich diet, staying hydrated, exercising regularly, avoiding tobacco, and limiting alcohol. Stress management and routine sleep are also crucial. Avoiding prolonged use of laxatives and NSAIDs helps protect the colon lining. Annual checkups and age-appropriate screenings ensure any developing colon problems are caught early and treated effectively.

Conclusion
Colon health is foundational to overall well-being, yet colon issues symptoms are often misunderstood, overlooked, or ignored until they escalate into serious conditions. From functional disorders like IBS to life-threatening diseases like colorectal cancer, the colon can reflect a wide spectrum of dysfunction—each with distinct causes, mechanisms, and implications. Understanding the early warning signs, exploring their potential sources, and pursuing evidence-based diagnostic and therapeutic pathways empowers both patients and healthcare providers to act with confidence and precision.
With advances in screening, diagnostics, and treatment, many colon problems are now highly manageable or even preventable. Timely recognition of colon problem symptoms, informed medical evaluation, and an integrative care strategy rooted in both science and empathy can restore health and quality of life.
As public awareness increases and stigma diminishes, more people are seeking preventive care and embracing lifestyle changes that promote colon resilience. The journey toward colon health begins with awareness, and it thrives on informed action. Whether you’re managing chronic symptoms, undergoing evaluation, or simply aiming for longevity, prioritizing your colon’s well-being is one of the most impactful steps you can take toward lifelong vitality.



