Introduction
The human body is an intricate network of systems, each with its own vital purpose—and among these, the gastrointestinal system stands out as a central pillar in maintaining overall health and wellness. Often referred to simply as the GI system, this complex series of organs is responsible for digesting food, absorbing nutrients, and eliminating waste. When something goes wrong within this system, the consequences can ripple throughout the body, leading to a wide range of symptoms and complications. This article explores the full scope of gastrointestinal health: what is a gastrointestinal condition, how the GI tract functions, and why gastrointestinal gastroenterology plays a pivotal role in diagnosing and managing these disorders.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
Understanding the basics of the GI system is essential for anyone looking to optimize their health, manage chronic issues, or simply recognize the early signs of digestive imbalance. From the esophagus to the rectum, every segment of the GI tract plays a unique and interconnected role. But what part of the GI tract does it affect when we feel bloated, experience acid reflux, or battle chronic constipation? These questions are more than just curiosities—they’re key to unlocking better digestive outcomes.
With increasing awareness around gut health, more individuals are seeking answers to terms like GI meaning medical or what is GI in medical terms. This article provides a comprehensive, EEAT-aligned guide that breaks down the gastrointestinal definition, explains how to define gastrointestinal health, and explores the systemic implications of GI conditions. Whether you’re new to the topic or navigating an existing diagnosis, understanding the fundamentals of gastrointestinal health is an empowering step toward improved well-being.

What Is the Gastrointestinal System?
The gastrointestinal system is the body’s central processing unit for all things food-related, comprising a long, continuous tube that starts at the mouth and ends at the anus. This system includes the oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus. Each organ plays a critical part in breaking down food, absorbing nutrients, and eliminating waste. Supplementary organs like the liver, pancreas, and gallbladder are also essential, aiding in enzymatic breakdown and nutrient processing.
When asking, what is a gastrointestinal system in everyday language, it’s essentially the infrastructure that transforms what we eat into the fuel our cells need to survive and thrive. In the medical community, GI stands for medical references to “gastrointestinal,” a term that denotes the stomach and intestine as well as the broader digestive tract. The gastrointestinal meaning is not limited to digestion alone—it encompasses immune function, hormonal balance, and even mental health, all of which are closely linked to gut health.
As food passes through each segment of the gastrointestinal system, it encounters enzymes, acids, and bacteria uniquely suited to that stage of digestion. Disruptions at any point—be it the esophagus or the colon—can have systemic effects. That’s why understanding what part of the GI tract does it affect when symptoms arise is crucial to accurate diagnosis and treatment.
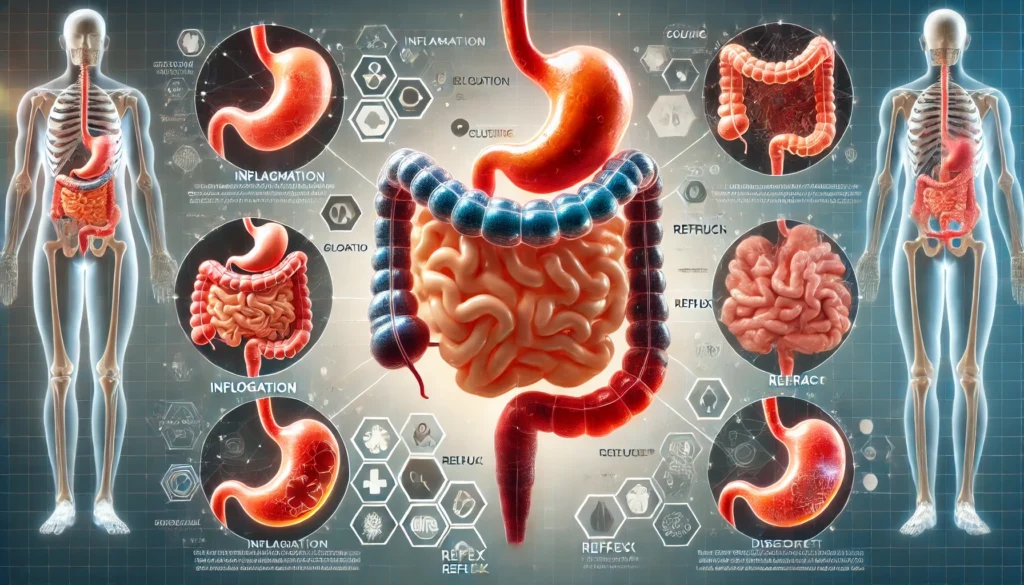
Common Gastrointestinal Conditions and Their Underlying Causes
Gastrointestinal conditions are among the most common medical complaints across the globe. They range from benign and temporary issues like indigestion to chronic and severe illnesses such as Crohn’s disease, ulcerative colitis, and gastrointestinal cancers. Understanding the gastrointestinal definition in a clinical context includes recognizing the spectrum of diseases that can affect this critical system.
Conditions like gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and peptic ulcers are functional or inflammatory issues that disrupt normal motility, secretion, and absorption. Infections caused by bacteria like Helicobacter pylori or viruses like norovirus also fall under this umbrella, as they target different areas of the gastrointestinal tract with varying symptoms.
When addressing what part of the GI tract does it affect, one must look at the condition in question. GERD, for instance, affects the lower esophageal sphincter and can lead to heartburn and regurgitation. IBS often targets the large intestine, causing bloating, gas, and irregular bowel habits. Understanding these distinctions is vital for determining the most appropriate interventions.
Contributing factors to gastrointestinal conditions can include poor dietary habits, chronic stress, sedentary lifestyles, smoking, alcohol use, infections, genetics, and autoimmune dysfunction. The gastrointestinal system is highly sensitive to inflammation and environmental toxins, making it vulnerable to a broad array of triggers.
GI Meaning Medical: Why Terminology Matters
In clinical settings, the abbreviation “GI” is ubiquitous. But for the average person, understanding the GI meaning medical terminology is essential to navigating doctor visits, treatment plans, and self-education. So what is GI in medical terms? GI stands for “gastrointestinal,” a compound term derived from “gastro” meaning stomach and “intestinal” meaning relating to the intestines.
The full gastrointestinal definition reflects not only the mechanical aspects of digestion but also the broader systemic roles the GI tract plays in immune surveillance, hormone regulation, and nutrient processing. Clarifying this terminology is essential for patients to be informed participants in their healthcare journey. This is especially true for those managing chronic GI conditions who frequently engage with gastrointestinal gastroenterology specialists.
Whether you’re reading a lab report or discussing symptoms with your provider, understanding terms like what is GI in medical terms or how to define gastrointestinal health enhances clarity and promotes better outcomes. It transforms patients from passive recipients of care to active health advocates.
Defining Gastrointestinal Function: More Than Digestion
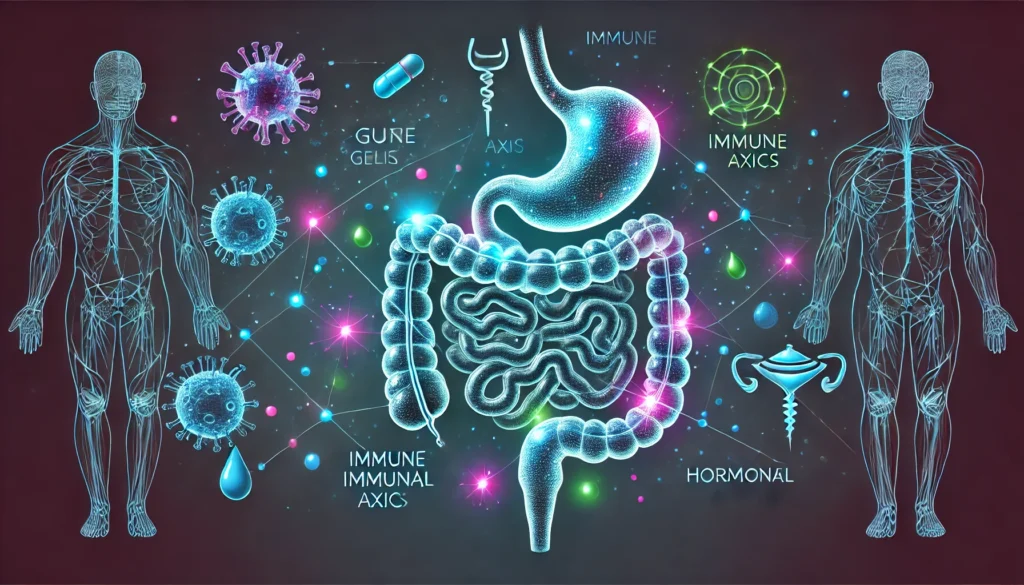
To define gastrointestinal function properly, one must go beyond the simplistic view of the digestive system as merely a conduit for food. Modern research emphasizes the GI tract as a complex, neuro-hormonal, and immune-responsive ecosystem. This perspective expands the gastrointestinal meaning to include roles in neurotransmitter production (like serotonin), immune function, and microbiome balance.
For example, the small intestine isn’t just responsible for nutrient absorption; it’s also where the majority of the immune system resides in the form of gut-associated lymphoid tissue (GALT). This makes it a frontline defense against pathogens. The colon, often overlooked, is home to trillions of bacteria that ferment undigested carbohydrates, produce short-chain fatty acids, and contribute to mood regulation.
Understanding what part of the GI tract does it affect when symptoms occur can reveal underlying dysfunctions that have far-reaching effects beyond digestion. Constipation may signal dysbiosis in the colon, while nutrient deficiencies could indicate issues in the small intestine. Each part of the gastrointestinal system provides valuable diagnostic clues.
This is why it is crucial to move beyond narrow definitions and embrace a systems-based approach. Defining gastrointestinal health means evaluating gut barrier integrity, microbial diversity, enzyme activity, and even vagus nerve function. Only by seeing the gastrointestinal tract in this holistic light can we truly assess and treat GI disorders effectively.
The Role of Gastrointestinal Gastroenterology in Diagnosis and Treatment
Gastroenterology is the branch of medicine focused on diagnosing, treating, and researching disorders of the gastrointestinal system. Practitioners in this field—known as gastroenterologists—are trained to handle a wide range of conditions, from acid reflux to colon cancer. Their expertise often begins where general practitioners’ knowledge ends, particularly when symptoms persist or escalate.
The discipline of gastrointestinal gastroenterology bridges clinical observation with advanced diagnostic techniques. Colonoscopies, endoscopies, capsule endoscopy, and biopsies are just a few of the tools used to visualize and assess what part of the GI tract does it affect when a disorder is suspected. Blood tests, stool analyses, and imaging studies complement these investigations to provide a comprehensive picture.
Gastroenterologists also play a vital role in patient education, helping individuals understand the GI meaning medical terminology that often appears in diagnostic summaries and reports. By demystifying terms like gastrointestinal definition or what is GI in medical terms, they foster better communication and collaboration.
Importantly, treatment protocols in gastroenterology often combine pharmacological, dietary, behavioral, and surgical strategies. This multi-pronged approach is essential because many GI conditions are multifactorial. Managing Crohn’s disease, for example, may involve immunosuppressants, dietary adjustments, stress reduction techniques, and sometimes surgical interventions.
The Microbiome and Gastrointestinal Health
In recent years, scientific interest in the human microbiome has surged—and for good reason. The gut is home to trillions of microbes that form an ecosystem essential for metabolic, immune, and neurological health. This biological universe further expands the gastrointestinal definition by including interactions between host and microbiota.
Microbial imbalances—known as dysbiosis—have been linked to a wide range of gastrointestinal conditions, including IBS, inflammatory bowel disease, and even colorectal cancer. Understanding the gut’s microbial landscape helps clarify what is a gastrointestinal dysfunction at its root cause rather than merely managing symptoms.
The GI tract also communicates with the brain via the gut-brain axis, a bidirectional system involving neurotransmitters, vagal pathways, and immune mediators. This connection offers insights into why anxiety, depression, and cognitive fog often accompany gastrointestinal issues.
Microbiome testing, probiotic and prebiotic interventions, and fermented food strategies are increasingly incorporated into integrative treatment models. All of this reinforces why gastrointestinal gastroenterology must now incorporate microbiological and neurological insights to remain effective and evidence-based.
Chronic Inflammation and the GI Tract
One of the most destructive forces within the gastrointestinal system is chronic inflammation. While acute inflammation is a protective response to injury or infection, chronic inflammation can erode gut lining, disrupt microbial balance, and trigger autoimmune responses. Conditions like Crohn’s disease and ulcerative colitis are characterized by persistent inflammation that damages the bowel wall and impairs function.
So what part of the GI tract does it affect in these cases? With Crohn’s disease, inflammation can affect any part of the gastrointestinal tract, from mouth to anus, although it most commonly targets the ileum. Ulcerative colitis, in contrast, is typically restricted to the colon and rectum. The inflammation in both conditions causes symptoms like abdominal pain, bloody stools, weight loss, and fatigue.
Anti-inflammatory medications, immunomodulators, biologics, and lifestyle interventions are essential for managing these diseases. Patients must work closely with gastrointestinal gastroenterology professionals to tailor treatment plans that reduce inflammation while preserving gut integrity and function.
Understanding the inflammatory basis of these diseases helps broaden the discussion beyond symptom control to include root cause resolution. This aligns with EEAT principles, encouraging patients and providers to adopt a systems-based, evidence-informed approach to care.
Nutritional Impacts on the Gastrointestinal System
Diet is perhaps the most controllable factor influencing gastrointestinal health. The foods we consume affect digestion, microbial composition, motility, and nutrient availability. Yet despite this, nutrition is often underemphasized in conventional GI treatment plans.
Defining gastrointestinal wellness must therefore include a dietary assessment. For instance, fiber-rich diets promote motility and microbial diversity, while highly processed foods can foster inflammation and dysbiosis. Elimination diets, low FODMAP protocols, and tailored reintroduction plans can significantly alleviate symptoms for patients with IBS or food sensitivities.
In conditions like celiac disease, removing gluten entirely is essential to prevent autoimmune responses. In IBD cases, certain carbohydrates may exacerbate inflammation, while omega-3 fatty acids and curcumin have shown promise in reducing inflammatory markers.
Hydration, meal timing, and food combinations also impact the gastrointestinal system’s efficiency. Proper chewing, stress reduction during meals, and mindful eating enhance enzymatic activity and nutrient uptake. This holistic approach to diet aligns with integrative gastroenterology models that treat the whole person—not just the disease.

Frequently Asked Questions
1. What is a gastrointestinal condition and how is it diagnosed?
A gastrointestinal condition refers to any disorder that affects the digestive tract, including the esophagus, stomach, intestines, liver, pancreas, or gallbladder. These conditions can range from temporary and mild, such as indigestion, to chronic and severe, like Crohn’s disease or colon cancer. Diagnosis usually involves a combination of clinical history, physical examination, lab tests, and diagnostic imaging such as endoscopy, colonoscopy, or CT scans. Gastroenterologists may also utilize stool analysis, pH monitoring, or breath tests to gather deeper insights. Early and accurate diagnosis is crucial because gastrointestinal symptoms often overlap, and misdiagnosis can lead to ineffective treatment.
2. What is GI in medical terms and why is it important to understand?
In medical terms, GI stands for gastrointestinal, a term that encompasses the entire digestive tract. Understanding what is GI in medical terms helps patients navigate healthcare more effectively. The GI tract plays a role not only in digestion but also in immune response, hormonal regulation, and neurological signaling. Being familiar with this terminology empowers patients to understand their test results, engage in informed conversations with their healthcare providers, and actively participate in treatment planning. This knowledge is foundational to improving digestive health and making well-informed lifestyle choices.
3. What part of the GI tract does it affect when someone experiences acid reflux?
When someone experiences acid reflux, the part of the GI tract affected is typically the lower esophageal sphincter, a ring of muscle between the esophagus and stomach. If this sphincter weakens or relaxes inappropriately, stomach acid can flow back into the esophagus, leading to burning sensations, chest pain, and even chronic cough. This condition is known as gastroesophageal reflux disease (GERD) when it becomes chronic. Treatment may include dietary changes, medications to reduce stomach acid, and in severe cases, surgical interventions. Understanding this specific anatomical focus helps in tailoring effective and targeted therapies.
4. How do you define gastrointestinal health from a modern medical perspective?
To define gastrointestinal health today involves more than just the absence of digestive symptoms. Modern medicine considers GI health a composite of efficient digestion, balanced microbiota, intact gut lining, healthy motility, and minimal inflammation. It also includes the GI tract’s ability to support immunity and hormone regulation. An individual may have regular bowel movements but still suffer from subtle GI dysfunctions such as poor nutrient absorption or microbial imbalance. Comprehensive GI health evaluations often include lab testing, dietary assessment, and a symptom inventory to uncover root causes of imbalance.
5. What is the gastrointestinal system’s role beyond digestion?
The gastrointestinal system is essential for digestion, but its influence extends far beyond. It plays a critical role in immune system regulation, with nearly 70% of immune cells residing in the gut. The GI tract also affects brain function via the gut-brain axis, which includes signaling pathways that influence mood, cognition, and mental health. Additionally, the GI system helps regulate hormones such as ghrelin and leptin, which control hunger and satiety. This systemic influence makes it clear that any disruption in GI health can manifest as far-reaching physical and emotional symptoms.
6. What does the term “gastrointestinal gastroenterology” refer to?
Gastrointestinal gastroenterology refers to the medical specialty focused specifically on diseases and disorders of the digestive system. This includes diagnosis, treatment, and prevention of conditions affecting the esophagus, stomach, intestines, pancreas, liver, and gallbladder. Gastroenterologists are experts trained to use diagnostic tools like endoscopies and colonoscopies and to interpret complex lab and imaging data. The term underscores the field’s dual focus on both structure and function within the digestive system. Understanding the role of gastroenterology is key for managing chronic conditions and for preventive screening, such as colon cancer checks.
7. Why is understanding “GI stands for medical” relevant in everyday healthcare?
Understanding that GI stands for medical terminology relating to the gastrointestinal system is crucial for interpreting clinical discussions, health articles, and treatment recommendations. As GI-related symptoms are among the most frequently reported health issues, knowing what GI means allows patients to better understand diagnoses, participate in decision-making, and follow medical instructions. This foundational knowledge also supports public health literacy and promotes more effective communication between patients and providers, which is essential in a healthcare landscape increasingly focused on patient-centered care.
8. Can the gastrointestinal tract affect mental health?
Yes, the gastrointestinal tract has a significant impact on mental health through what is known as the gut-brain axis. This bidirectional communication pathway connects the emotional and cognitive centers of the brain with intestinal functions. A large percentage of the body’s serotonin is produced in the GI tract, and microbial imbalances have been linked to mood disorders like depression and anxiety. Chronic inflammation in the gut can also affect neurochemical balance and lead to symptoms such as brain fog or low energy. Supporting gut health is thus an emerging strategy in integrative approaches to mental health care.
9. What is the difference between the terms “gastrointestinal definition” and “gastrointestinal meaning”?
While the terms “gastrointestinal definition” and “gastrointestinal meaning” are often used interchangeably, they serve slightly different functions. The gastrointestinal definition typically refers to the formal, medical description of the system—including its anatomy, physiology, and function. The gastrointestinal meaning, on the other hand, may encompass its practical implications, such as how it relates to overall health, disease risk, and daily functioning. Understanding both enhances comprehension and helps bridge the gap between clinical terminology and lived experience, allowing patients to take more proactive roles in their care.
10. How can I maintain a healthy gastrointestinal system?
Maintaining a healthy gastrointestinal system involves several lifestyle and dietary strategies. Eating a fiber-rich diet, staying hydrated, and minimizing processed foods support healthy digestion and microbiome diversity. Regular physical activity aids motility and reduces inflammation. Managing stress is also crucial, as chronic stress can alter gut flora and impair digestion. Routine medical checkups and screenings, especially if there’s a family history of GI disorders, are important for early detection and intervention. Probiotic and prebiotic foods, as well as mindful eating habits, also contribute to long-term gastrointestinal wellness.

Conclusion
The gastrointestinal system is far more than a digestive machine—it is a complex, dynamic hub of metabolic, immunologic, and neurological activity. Understanding what is a gastrointestinal condition, how to define gastrointestinal function, and what part of the GI tract does it affect during illness or imbalance equips individuals to take control of their health in more meaningful ways. As patients become increasingly empowered and healthcare shifts toward integrative, personalized models, the importance of gastrointestinal gastroenterology only continues to grow.
The terms GI meaning medical and what is GI in medical terms may seem like technical jargon at first, but they are gateways to deeper health literacy. When individuals understand the gastrointestinal definition and how their own system functions, they can make choices that foster long-term vitality. This includes everything from dietary adjustments and stress management to regular screenings and evidence-based treatments.
Ultimately, gut health is whole-body health. Through ongoing research, clinical excellence, and informed self-care, the gastrointestinal system can be supported in ways that benefit every other system in the body. Whether you’re just learning about digestive health or managing a chronic condition, embracing this knowledge is a powerful step toward a better, more resilient life.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Sudden Uncontrollable Diarrhea and Loose Feces: Causes, Risks, and Effective Scientific Treatments



