Introduction
The upper digestive system is an intricate and vital component of human health, responsible for the initial stages of digestion and the absorption of nutrients critical for bodily function. When this delicate system malfunctions, it can lead to discomfort, chronic illness, and diminished quality of life. Upper digestive tract issues are not only prevalent but often misunderstood, leading to misdiagnosis, inadequate treatment, and prolonged suffering for millions around the globe. Whether manifesting as mild heartburn, chronic nausea, or severe inflammation, these problems deserve focused attention from both patients and healthcare providers.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
The umbrella of upper gastrointestinal issues includes a wide range of disorders—some structural, others functional—that affect areas such as the esophagus, stomach, and duodenum. Conditions like acid reflux, peptic ulcers, gastroparesis, and esophageal motility disorders often present overlapping symptoms that can mask their root causes, making diagnosis a significant clinical challenge. Furthermore, lifestyle choices, medications, and even psychological stress are increasingly recognized as contributing factors to upper digestive problems, often in ways not traditionally acknowledged by conventional medicine.
Understanding the nature, mechanisms, and triggers of these disorders is essential to devising effective treatment plans and long-term management strategies. With increasing scientific attention on the gut-brain axis and microbiome health, new research has begun to reshape how we interpret digestive distress, linking physical symptoms to neurological and systemic factors. This comprehensive article explores the causes, symptoms, diagnostics, and evidence-based treatment of upper GI issues, offering clarity, medical accuracy, and holistic strategies grounded in current science.
For anyone suffering from persistent digestive discomfort or looking to understand what upper gastrointestinal health truly entails, this exploration into upper GI tract problems provides a foundational resource rooted in expertise, trust, and actionable insights.

Understanding the Anatomy and Function of the Upper GI Tract
The upper gastrointestinal tract begins at the mouth and extends through the esophagus, stomach, and the first portion of the small intestine known as the duodenum. This part of the digestive system is tasked with the ingestion, mechanical breakdown, chemical processing, and early absorption of food and liquids. Salivary enzymes begin digestion in the mouth, but it is within the stomach and duodenum that complex macronutrients are further broken down into absorbable components.
The esophagus serves as the muscular tube connecting the throat to the stomach. When functioning normally, it propels swallowed food downward via a coordinated series of muscular contractions called peristalsis. A circular muscle at the lower end, the lower esophageal sphincter (LES), opens to allow food into the stomach and then closes to prevent acidic stomach contents from refluxing upward.
In the stomach, powerful gastric acids and enzymes break down proteins and further liquefy food. The stomach lining, protected by mucus, withstands this acidic environment. Next, the chyme—a semi-fluid mixture of digested food—moves into the duodenum, where it meets bile from the liver and enzymes from the pancreas, enabling further digestion and nutrient absorption.
When any part of this system is disrupted, upper digestive tract issues can arise. Problems such as acid reflux, ulcers, and gastric emptying disorders may develop due to mechanical obstruction, inflammatory disease, muscular dysfunction, or chemical imbalances. Understanding this anatomy is crucial for identifying the origins of upper GI problems and providing specific, targeted therapies.
The Most Common Upper GI Issues: Diagnosis and Distinction
Upper GI problems manifest in several common but clinically distinct disorders. Gastroesophageal reflux disease (GERD), peptic ulcer disease, gastritis, functional dyspepsia, and gastroparesis are among the most frequently reported. Though these disorders share some overlapping symptoms such as pain, bloating, nausea, or regurgitation, their pathophysiological underpinnings differ.
GERD is primarily characterized by acid reflux due to a weakened or malfunctioning LES. It may result from hiatal hernia, obesity, pregnancy, or lifestyle triggers such as caffeine and alcohol. Peptic ulcers, by contrast, are erosions in the gastric or duodenal lining, often caused by Helicobacter pylori infection or long-term NSAID use.
Functional dyspepsia is a diagnosis of exclusion when no anatomical cause is found but symptoms like early satiety, bloating, and upper abdominal discomfort persist. Gastroparesis involves delayed gastric emptying due to nerve or muscle dysfunction, commonly seen in diabetics and patients with vagus nerve damage.
It is critical to accurately distinguish between these conditions, as misdiagnosis can lead to inappropriate treatments and worsening of symptoms. Diagnostic procedures may include upper endoscopy, pH monitoring, gastric emptying studies, and H. pylori testing. Understanding the specific nature of the disorder is the first step toward resolving upper digestive problems effectively.

Causes and Risk Factors of Upper Digestive Tract Issues
There is no single cause of upper digestive tract issues. These disorders result from a complex interplay of genetic predispositions, environmental exposures, microbiome imbalances, and lifestyle factors. One of the most common triggers is diet—specifically, the consumption of fatty, spicy, or acidic foods that irritate the gastric lining or increase stomach acid production. Smoking, alcohol intake, and high caffeine consumption further compound these effects.
Stress has a substantial impact on upper gastrointestinal function. Through the gut-brain axis, psychological tension can disrupt motility, increase acid secretion, and reduce mucosal blood flow, making the digestive lining more vulnerable to damage. Chronic stress is also linked to dysbiosis, where the balance of healthy gut bacteria is altered, influencing inflammation and immune response.
Medications such as NSAIDs (ibuprofen, aspirin), corticosteroids, and certain antibiotics are well-known for their role in upper GI problems, particularly in the development of ulcers and gastritis. Long-term proton pump inhibitor (PPI) use, while relieving GERD symptoms, may paradoxically increase risk for some upper GI tract problems by altering the natural stomach acid environment and microbiota.
Age, genetics, infections (notably H. pylori), and chronic diseases such as diabetes or autoimmune conditions also elevate the risk of upper gastrointestinal issues. Understanding these multifactorial triggers enables clinicians and patients to implement preventive strategies and make informed therapeutic decisions.
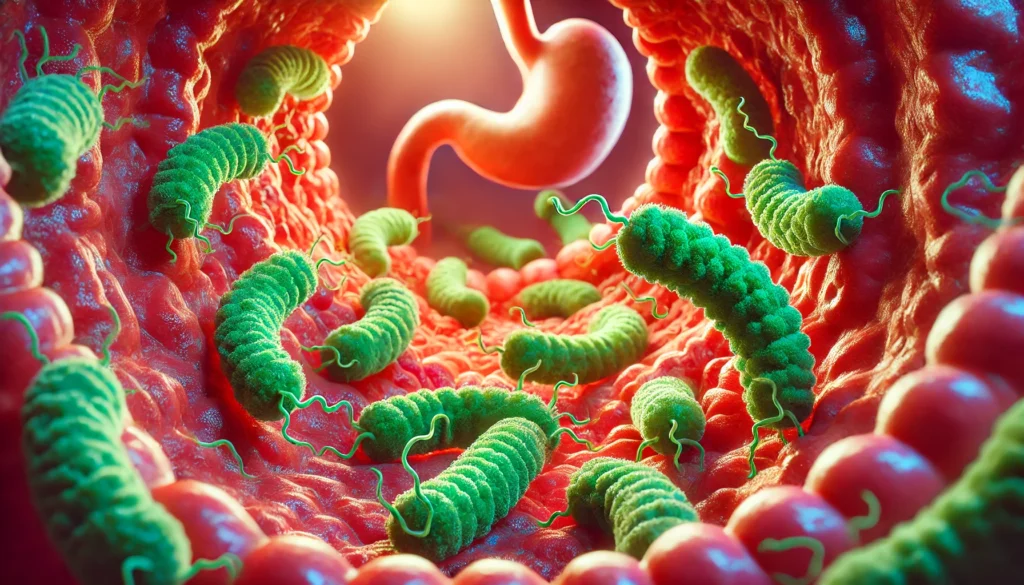
The Role of Helicobacter Pylori in Upper GI Problems
Helicobacter pylori is a spiral-shaped bacterium that colonizes the stomach lining and plays a central role in many upper gastrointestinal issues. Its presence has been strongly associated with chronic gastritis, peptic ulcers, and even gastric cancer. H. pylori infection affects roughly half the global population, although not all carriers develop symptoms or disease.
The bacterium survives the harsh acidic environment of the stomach by producing urease, an enzyme that neutralizes gastric acid. In doing so, it damages the protective mucosal lining and triggers an inflammatory response. Over time, this process may lead to erosion of the stomach or duodenal lining, resulting in ulcers.
Diagnosing H. pylori involves a combination of urea breath tests, stool antigen tests, blood antibody screening, or gastric biopsy during endoscopy. Once confirmed, treatment typically involves triple or quadruple therapy: a combination of two or more antibiotics along with acid-suppressing medications like PPIs.
Although H. pylori is a known culprit in many upper GI problems, its presence is not always harmful. Emerging research suggests it may play a role in regulating stomach hormones and microbiota composition, underscoring the need for nuanced, evidence-based treatment decisions rather than blanket eradication.
Symptoms That Signal Upper Gastrointestinal Issues
Symptoms of upper digestive problems vary widely depending on the specific disorder, yet certain patterns provide valuable clues. Heartburn and acid regurgitation are hallmark symptoms of GERD, particularly when aggravated by meals or lying down. In contrast, gnawing or burning pain that improves after eating may indicate a duodenal ulcer, whereas pain that worsens with food intake suggests a gastric ulcer.
Nausea, early satiety, and bloating are common to both gastroparesis and functional dyspepsia, making diagnosis challenging. Belching, hiccups, and a feeling of fullness even after small meals often accompany these symptoms. In some cases, vomiting undigested food hours after eating is a telltale sign of delayed gastric emptying.
Unexplained weight loss, anemia, or gastrointestinal bleeding (evidenced by black stools or vomiting blood) should raise concern for more serious conditions such as gastric malignancy or severe ulceration. Persistent or worsening symptoms demand prompt medical evaluation, as delays in diagnosis can lead to complications and reduced treatment efficacy.
Diagnostic Tools for Identifying Upper GI Tract Problems
Accurate diagnosis of upper digestive problems requires a combination of clinical assessment, patient history, and specialized diagnostic tests. Upper endoscopy, or esophagogastroduodenoscopy (EGD), remains the gold standard for visualizing the esophagus, stomach, and duodenum directly. It allows for biopsy, detection of ulcers, inflammation, tumors, and other abnormalities.
Barium swallow radiographs can reveal structural anomalies such as strictures, hiatal hernias, or esophageal diverticula. Ambulatory pH monitoring measures acid exposure in the esophagus over 24 hours, providing insight into reflux severity and correlation with symptoms.
Gastric emptying scintigraphy assesses the speed at which food leaves the stomach, essential in diagnosing gastroparesis. Breath tests and stool analysis are crucial for detecting H. pylori infections. In some cases, esophageal manometry may be used to evaluate muscle contractions and sphincter function, especially in patients with suspected motility disorders.
Choosing the right diagnostic tool depends on the patient’s symptoms, risk factors, and previous treatment responses. Personalized diagnostics are essential to avoid unnecessary procedures and guide effective therapy for upper GI issues.
Evidence-Based Treatments for Upper Digestive Tract Disorders
Effective treatment of upper gastrointestinal issues depends on the underlying cause, symptom severity, and individual patient factors. Acid suppression is a cornerstone of therapy for GERD, ulcers, and gastritis. Proton pump inhibitors (PPIs) such as omeprazole or esomeprazole are commonly prescribed to reduce acid secretion and promote healing. H2 receptor blockers and antacids may be used for milder symptoms or in combination therapy.
When H. pylori is involved, eradication regimens using multiple antibiotics are essential, followed by re-testing to confirm success. For patients with functional disorders such as dyspepsia or gastroparesis, treatment often includes prokinetic agents like metoclopramide to enhance gastric motility.
Dietary modification plays a vital role. Patients are advised to avoid triggers such as fatty foods, alcohol, caffeine, and late-night meals. Small, frequent meals and elevated sleeping positions can alleviate GERD symptoms. In gastroparesis, low-fiber, low-fat diets that are easier to digest are often recommended.
Psychological interventions, including cognitive-behavioral therapy and stress management, can significantly benefit patients whose symptoms are exacerbated by anxiety or depression. In refractory cases, surgical interventions such as fundoplication for GERD or gastric electrical stimulation for gastroparesis may be considered.
Emerging therapies, including gut-directed hypnotherapy, neuromodulators, and microbiome-based treatments, offer new hope for complex upper GI tract problems, particularly when conventional options fail to provide relief.
The Importance of Diet and Lifestyle in Managing Upper GI Issues
Nutrition and lifestyle choices are integral to managing upper digestive problems. While medications can provide relief, long-term resolution often requires addressing behavioral and dietary contributors. Individuals with upper digestive tract issues benefit from a tailored diet plan that minimizes trigger foods and promotes gut healing.
Avoiding large meals, eating slowly, and chewing thoroughly can prevent bloating and reflux. Foods high in fat, chocolate, spicy ingredients, onions, citrus, and carbonated beverages are common aggravators. A Mediterranean-style diet rich in fiber, lean proteins, and anti-inflammatory compounds has shown promise in improving GI function and reducing symptoms.
Lifestyle adjustments such as weight loss, smoking cessation, regular physical activity, and adequate hydration are also vital. These measures not only alleviate existing symptoms but also reduce the risk of developing chronic upper gastrointestinal issues.
Mindful eating practices, including attention to hunger and fullness cues and avoiding emotional eating, help address functional symptoms often linked to stress and anxiety. Consistency in meal timing and improved sleep hygiene further support digestive health and circadian alignment.
The interplay between lifestyle, diet, and upper GI health underscores the importance of a holistic treatment approach, empowering patients to take an active role in their healing process.
Frequently Asked Questions
1. What is considered the upper digestive tract, and why is it so important?
The upper digestive tract includes the esophagus, stomach, and the beginning of the small intestine, known as the duodenum. This region is critical for initiating digestion, breaking down food, and preparing nutrients for absorption. It also plays a major role in regulating appetite, hormones, and immune responses through the gut-brain axis. When this part of the GI system is compromised, it can lead to upper digestive tract issues that affect not only digestion but also overall well-being, energy levels, and nutrient balance.
2. How are upper GI issues different from lower GI problems?
Upper GI problems involve the esophagus, stomach, and duodenum, whereas lower GI problems affect the small intestine beyond the duodenum, the colon, rectum, and anus. Symptoms of upper GI issues often include heartburn, nausea, vomiting, and upper abdominal pain, while lower GI disorders may cause bloating, constipation, diarrhea, and lower abdominal discomfort. Differentiating between the two helps doctors tailor diagnostic tools and treatments for the specific part of the digestive system involved.
3. Can stress really cause upper digestive problems?
Yes, stress has a significant impact on upper gastrointestinal function. It affects motility, acid production, and the gut microbiome, contributing to symptoms like indigestion, reflux, and stomach pain. Chronic stress can also impair the protective lining of the stomach, making it more vulnerable to inflammation and ulcers. Managing stress through behavioral therapy, relaxation techniques, and physical activity can play a crucial role in reducing the severity and frequency of upper digestive problems.
4. Are upper gastrointestinal issues permanent, or can they be cured?
The prognosis for upper GI tract problems varies depending on the specific condition. Many issues, such as GERD, gastritis, and ulcers, can be effectively treated and even cured with medications, dietary changes, and eradication of underlying infections like H. pylori. However, chronic conditions such as gastroparesis or functional dyspepsia may require long-term management. Early diagnosis and personalized treatment plans significantly improve outcomes and quality of life for individuals with upper digestive tract issues.
5. What role does the microbiome play in upper GI health?
The gut microbiome is a diverse ecosystem of microorganisms that influence digestive processes, immunity, and inflammation. Although much of the microbiome resides in the colon, the upper GI tract also hosts bacterial populations that can impact health. Imbalances or overgrowths in this region are associated with conditions like SIBO (small intestinal bacterial overgrowth) and upper digestive problems like bloating, nausea, and pain. Probiotic and prebiotic therapies, along with diet changes, are increasingly being used to support microbiome balance and treat upper gastrointestinal issues.
6. Can food allergies or intolerances cause upper GI tract problems?
Yes, food intolerances and allergies can cause a range of upper GI symptoms including acid reflux, nausea, and stomach pain. Lactose intolerance, gluten sensitivity, and allergies to specific proteins can irritate the gastric mucosa or alter motility. In some individuals, eating trigger foods leads to immediate discomfort or delayed symptoms that mimic common upper digestive tract issues. Identifying and eliminating these foods through testing and elimination diets can lead to significant symptom relief and digestive healing.
7. Why do upper GI problems often recur even after treatment?
Recurrence of upper GI issues may occur due to incomplete treatment, poor adherence to lifestyle changes, re-infection (in the case of H. pylori), or underlying chronic conditions that were not addressed. Some medications relieve symptoms but do not cure the root cause. Stress, diet, and behavioral habits also contribute to the reappearance of symptoms. A comprehensive treatment plan that includes follow-up care, behavioral support, and dietary counseling can significantly reduce the likelihood of recurrence.
8. What’s the difference between acid reflux and GERD?
Acid reflux refers to the occasional backflow of stomach acid into the esophagus, causing heartburn. When this occurs frequently and disrupts daily life, it may be diagnosed as gastroesophageal reflux disease (GERD). GERD is a chronic, more severe form of reflux that can lead to complications like esophagitis, Barrett’s esophagus, or even esophageal cancer. Understanding this distinction is key for choosing the right treatments and avoiding long-term damage from untreated upper GI issues.
9. Can children or young adults suffer from upper GI tract problems?
Absolutely. While upper gastrointestinal issues are more common in adults, children and young adults can also experience conditions like GERD, gastritis, and even ulcers. Poor dietary habits, stress from school, infections, and genetics can all contribute. Pediatric upper GI problems may present differently and are sometimes overlooked or mistaken for behavioral issues. Timely evaluation by a pediatric gastroenterologist is essential when symptoms persist in younger populations.
10. Are natural or alternative treatments effective for upper digestive problems?
Many individuals find relief through natural or integrative approaches, including dietary modifications, herbal supplements, and mind-body therapies. Ginger, licorice root, slippery elm, and chamomile have been studied for their soothing effects on the stomach lining and ability to reduce inflammation. Acupuncture, yoga, and gut-directed hypnotherapy have shown promise in functional GI disorders. However, it’s vital to consult healthcare professionals before starting any alternative treatment, especially when symptoms are severe or persistent.

Conclusion
Upper gastrointestinal issues are a prevalent and often under-recognized category of digestive disorders that can significantly affect quality of life and overall health. From common problems like GERD and peptic ulcers to complex conditions such as gastroparesis or functional dyspepsia, upper digestive tract issues arise from a mix of anatomical, biochemical, microbial, and lifestyle-related factors. Comprehensive understanding and timely intervention are crucial to preventing complications, alleviating discomfort, and promoting long-term digestive health.
Through a combination of evidence-based treatments, dietary modifications, lifestyle changes, and, when needed, medical procedures, most upper GI problems can be effectively managed or resolved. The importance of accurate diagnosis and personalized care cannot be overstated, as each condition carries unique characteristics that demand tailored approaches. Advances in diagnostic tools, microbiome research, and gut-brain communication are paving the way for more precise and holistic therapies.
Whether one is experiencing mild discomfort or chronic symptoms, recognizing the significance of upper digestive health and seeking expert evaluation is the first step toward healing. Informed decisions grounded in science, combined with empowered self-care, can transform the management of upper gastrointestinal issues into a journey of restoration, resilience, and renewed well-being.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Gastrointestinal Disease: New Diagnostic and Therapeutic Approaches



