Introduction
Functional gastrointestinal disorders have become an increasingly prominent subject in both clinical research and everyday health discussions, affecting millions of individuals around the world who struggle with chronic digestive symptoms despite normal diagnostic results. These disorders often leave patients frustrated and misunderstood, as they experience real discomfort without any identifiable structural or biochemical cause upon standard medical examination. The conditions are not imaginary or psychosomatic—they are biological, rooted in complex physiological processes involving the gut, brain, immune system, and microbiota.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
The term “functional” in this context refers to the altered functioning of the gastrointestinal (GI) tract rather than any visible pathology. This includes abnormalities in motility, visceral sensitivity, immune activation, gut permeability, and neural regulation. Collectively referred to as functional GI disorders, these conditions include irritable bowel syndrome (IBS), functional dyspepsia, functional bloating, functional constipation, and other symptom-defined syndromes that profoundly affect quality of life.
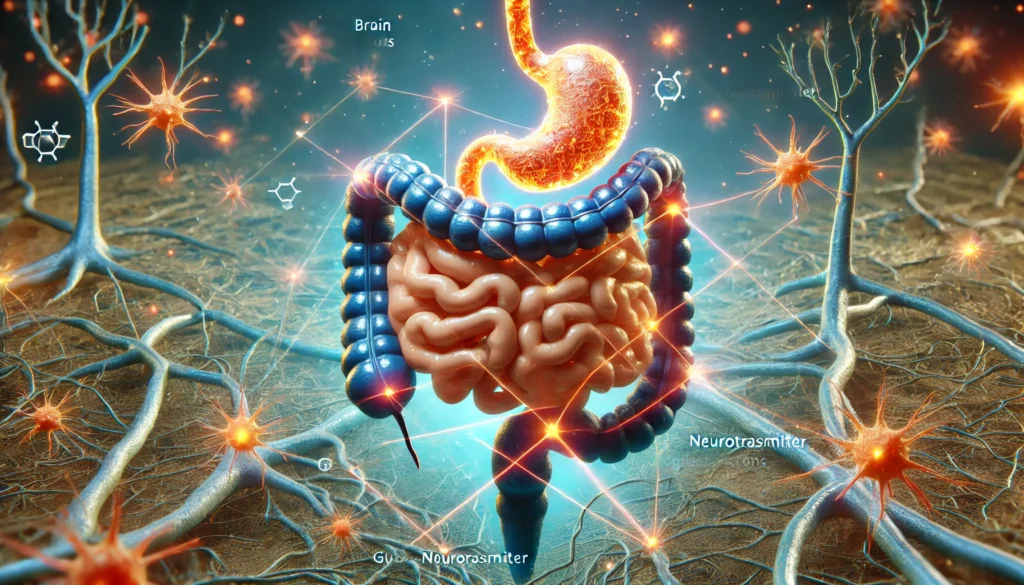
It is now widely accepted that functional gastrointestinal disorders are linked to disruptions in the gut-brain axis—a complex communication system that integrates emotional, cognitive, hormonal, and microbial signals to regulate digestive function. Patients with functional GI issues often report a strong association between stress, emotional disturbances, and symptom flare-ups, which reflects this intricate physiological connection.
Understanding and managing functional GI disorders requires a shift in both medical thinking and patient care. Traditional tests may not reveal obvious abnormalities, but newer insights into gut-brain interactions, intestinal barrier dysfunction, low-grade inflammation, and microbial dysbiosis are illuminating the biological underpinnings of these chronic conditions. This article provides a deep exploration of the causes, mechanisms, clinical presentation, diagnostic strategies, and evidence-backed treatments for these multifaceted disorders, adhering to EEAT (Experience, Expertise, Authoritativeness, and Trustworthiness) principles throughout. Whether you are a patient searching for answers or a practitioner seeking clarity, this guide serves as a comprehensive resource grounded in science and compassion.

What Are Functional GI Disorders?
Functional gastrointestinal disorders are a group of chronic digestive conditions characterized by recurring symptoms that cannot be attributed to structural abnormalities, infections, or systemic illnesses. Instead of detectable tissue damage or biochemical changes, these disorders stem from functional irregularities in how the GI tract behaves and communicates with the nervous system. Despite a lack of visible damage on diagnostic imaging or endoscopy, patients experience a wide range of symptoms—from cramping and bloating to altered bowel movements and nausea—that can be severe and persistent.
The Rome IV criteria serve as the globally accepted diagnostic framework for these disorders, allowing clinicians to classify them based on symptom patterns, duration, and impact on daily functioning. Under this classification, functional gastrointestinal disorders are divided according to the region of the GI tract they affect. For example, functional gastric disorders impact the upper GI tract, including the stomach and duodenum, while functional GI disorders such as IBS affect the lower digestive tract, including the small and large intestines.
Unlike traditional GI diseases like ulcers, Crohn’s disease, or colorectal cancer, which show up clearly on tests, functional GI conditions present diagnostic and therapeutic challenges. This makes it all the more important to understand their defining features, so that appropriate treatment pathways can be developed for each unique patient.
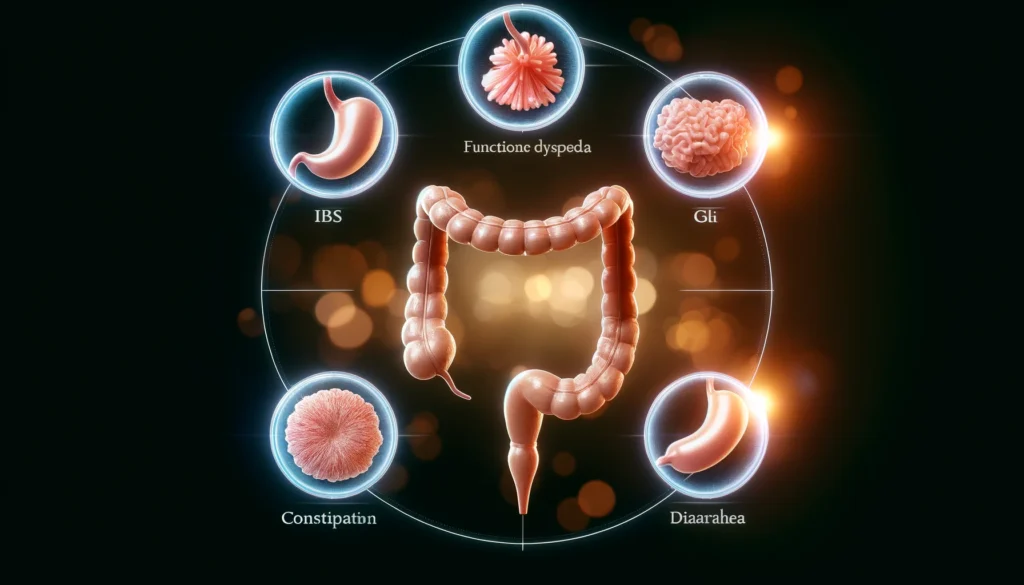
Types of Functional Gastrointestinal Disorders
Functional GI disorders can affect any part of the digestive system and are often categorized by the primary symptom or location of discomfort. The five most commonly diagnosed forms are as follows:
Irritable Bowel Syndrome (IBS):
A hallmark condition within the spectrum of functional GI disorders, IBS is marked by recurrent abdominal pain and changes in bowel habits—constipation, diarrhea, or a combination of both. Symptoms often worsen in response to stress or dietary triggers and can fluctuate in intensity over time.
Functional Dyspepsia:
This functional gastric disorder is characterized by persistent upper abdominal discomfort, early satiety, and a sense of fullness or burning unrelated to ulcers or reflux. It often affects the stomach’s ability to empty properly and may involve subtle inflammation of the gastric lining.
Functional Constipation:
In this condition, individuals experience infrequent, hard, or difficult-to-pass stools, along with feelings of incomplete evacuation. Unlike IBS, functional constipation does not typically involve abdominal pain as a central feature.
Functional Diarrhea:
Characterized by chronic loose or watery stools without the abdominal pain seen in IBS, this condition is another subset of functional gastrointestinal disorders with distinct diagnostic criteria under the Rome IV framework.
Functional Abdominal Bloating/Distension:
Many patients experience abdominal bloating or visible distension without other defining symptoms. These cases may involve impaired gas transit, visceral hypersensitivity, or disordered gut motility.
It’s not uncommon for patients to experience overlap between different types of functional GI disorders, making diagnosis and treatment even more complex. For instance, someone may suffer from both IBS and functional dyspepsia or shift between constipation and diarrhea over time. This fluidity in symptoms reflects the underlying dysfunction in regulatory pathways throughout the gastrointestinal system.
The Gut-Brain Axis and Its Role in Functional GI Disorders
Central to the pathophysiology of functional gastrointestinal disorders is the gut-brain axis—a sophisticated network that links the emotional and cognitive centers of the brain with enteric nerves that regulate digestion. This two-way communication system is mediated by neural circuits, hormones, immune signals, and gut microbiota, forming an integrated platform for gastrointestinal control.
In patients with functional GI disorders, disruptions in this axis can result in heightened visceral sensitivity, abnormal intestinal motility, and altered pain perception. Stress, anxiety, and trauma can intensify these signals, leading to cycles of symptom flares and psychological distress. Brain imaging studies have shown differences in pain processing and autonomic control in patients with IBS and functional gastric disorders, confirming that these are not “imagined” conditions but real physiological phenomena.
Neurotransmitters like serotonin and dopamine, which play a major role in mood and cognition, are also deeply involved in gut function. Over 90% of the body’s serotonin is produced in the GI tract, where it influences motility, secretion, and sensitivity. Dysregulation of serotonergic signaling has been implicated in both diarrhea-predominant and constipation-predominant IBS.
Understanding the gut-brain axis has revolutionized the treatment of functional gastrointestinal disorders, encouraging the use of mind-body therapies alongside dietary and pharmaceutical interventions. Gut-directed hypnotherapy, cognitive-behavioral therapy (CBT), mindfulness meditation, and antidepressant medications are now recognized as essential components of a comprehensive care plan.

Microbiota and Immune Factors in Functional GI Disorders
The intestinal microbiota—comprising trillions of bacteria, viruses, and fungi—plays a pivotal role in the regulation of gut function, immune tolerance, and inflammation. In individuals with functional GI disorders, alterations in microbial composition, known as dysbiosis, are frequently observed. These shifts can increase fermentation, gas production, and low-grade inflammation, leading to the typical symptoms of bloating, pain, and irregular stools.
Research has shown that patients with IBS have different microbial profiles compared to healthy individuals, including reduced diversity and altered levels of specific bacterial strains such as Firmicutes and Bacteroidetes. Some studies have linked functional gastric disorders with increased prevalence of Helicobacter pylori or small intestinal bacterial overgrowth (SIBO), although causality remains under investigation.
In addition to microbial changes, low-grade mucosal inflammation and immune activation are often present. Increased mast cell density near gut nerves, higher levels of pro-inflammatory cytokines, and impaired epithelial barrier function have all been documented in people with functional GI disorders. These findings support the theory that immune dysregulation and microbiota disturbances drive symptom development in many patients.
Probiotic and prebiotic therapies, antimicrobial protocols for SIBO, and anti-inflammatory supplements such as curcumin or glutamine are now being studied for their therapeutic potential in these disorders. By addressing the root causes of inflammation and microbial imbalance, clinicians can offer more effective and lasting relief for patients.
Frequently Asked Questions
1. What are the main symptoms of functional gastrointestinal disorders?
Symptoms vary depending on the specific disorder, but they often include abdominal pain, bloating, constipation, diarrhea, nausea, fullness after eating, and excessive gas. In functional gastric disorders, upper GI symptoms like early satiety and indigestion are more prominent, whereas lower GI disorders like IBS may involve frequent changes in bowel habits and cramping. These symptoms can fluctuate and are often influenced by stress, diet, and other environmental factors.
2. How is a functional GI disorder diagnosed?
Functional GI disorders are primarily diagnosed using Rome IV criteria, which classify conditions based on the pattern, frequency, and duration of symptoms. Diagnosis involves a detailed medical history, symptom questionnaires, and the exclusion of structural or inflammatory diseases through lab tests, imaging, and endoscopy. Specialized tools such as hydrogen breath testing for SIBO or anorectal manometry may be used when needed.
3. Are functional gastrointestinal disorders caused by stress?
Stress does not directly cause functional GI disorders, but it significantly contributes to symptom severity and frequency. Through the gut-brain axis, stress affects gut motility, increases intestinal permeability, alters microbiota composition, and enhances pain perception. Stress management strategies, including cognitive-behavioral therapy and relaxation techniques, have proven highly effective in reducing symptoms.
4. Can functional GI disorders be treated or cured?
While there is no universal cure, many individuals achieve symptom control and long-term improvement with the right combination of therapies. Treatment is often multifaceted, involving dietary changes, behavioral therapy, pharmacological agents, and gut microbiota support. The goal is to reduce symptom burden, restore function, and improve quality of life through personalized, evidence-based care.
5. What role does diet play in managing functional GI disorders?
Diet plays a crucial role in both symptom management and gut health. The low-FODMAP diet is particularly effective for IBS, reducing fermentable carbohydrates that fuel gas production and bloating. Elimination diets to identify food intolerances, as well as high-fiber or anti-inflammatory diets, can also be beneficial. Working with a dietitian ensures nutritional adequacy and personalized planning.
6. Are these disorders more common in women?
Yes, functional gastrointestinal disorders are more commonly reported in women than men. Hormonal fluctuations, particularly those involving estrogen and progesterone, may influence gut motility and pain sensitivity. Gender differences in stress response and brain-gut signaling may also contribute. Recognizing these differences is important for tailoring treatment approaches.
7. Is it possible to have more than one functional GI disorder?
Yes, symptom overlap is common, and many patients meet the criteria for more than one disorder. For example, a person may experience both functional dyspepsia and IBS, or alternate between constipation and diarrhea. This overlap requires a nuanced diagnostic approach and a flexible treatment plan that addresses all symptom dimensions.
8. What are functional gastric disorders specifically?
Functional gastric disorders refer to conditions like functional dyspepsia that primarily affect the stomach. Symptoms include post-meal fullness, early satiety, upper abdominal discomfort, and nausea. These disorders often involve delayed gastric emptying, hypersensitivity of stomach nerves, or subtle inflammation, and they typically require different treatment strategies than lower GI conditions.
9. Do functional GI disorders affect children?
Yes, children can suffer from functional abdominal pain, IBS, and functional dyspepsia. These conditions often manifest as school avoidance, reduced appetite, and mood disturbances. Pediatric treatment includes behavioral therapy, dietary adjustments, and family education. Early intervention can prevent chronicity and improve long-term outcomes.
10. What is the long-term outlook for someone with a functional GI disorder?
With appropriate and consistent care, many people experience significant symptom reduction or remission. Long-term outcomes depend on factors such as adherence to treatment, stress management, and co-existing conditions. Ongoing research is leading to more precise diagnostic tools and targeted therapies, offering hope for improved quality of life and long-term health.

Conclusion
Functional gastrointestinal disorders represent a challenging but increasingly understood area of digestive health. Once dismissed as stress-related or psychosomatic, these conditions are now recognized as complex neurogastroenterological syndromes with identifiable patterns of dysfunction in motility, sensitivity, immunity, and microbial balance. They affect millions globally, often interfering with daily life and emotional well-being, yet they are entirely manageable with modern, science-backed strategies.
From functional gastric disorders like dyspepsia to broader conditions like IBS, the key to effective management lies in an integrative, patient-centered approach. This includes accurate diagnosis through Rome IV criteria, exploration of gut-brain dynamics, dietary personalization, microbiota modulation, and psychological support. No two patients are alike, and the most successful interventions consider the whole person, not just their digestive tract.
Ongoing advances in microbiome science, neural imaging, and dietary therapeutics are rapidly transforming the field of functional gastroenterology. As understanding deepens, stigma fades, and awareness grows, patients can access better care, more empathetic support, and real symptom relief. By embracing both the complexity and the humanity of these disorders, clinicians and patients alike can walk a path of clarity, resilience, and healing—together.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Functional gastrointestinal disorders: advances in understanding and management
Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features, and Rome IV



