Introduction
Digestive distress is one of the most common and disruptive health concerns affecting individuals worldwide, and yet, the intricate and often confusing nature of gastrointestinal symptoms makes it incredibly difficult to diagnose and treat effectively. If you’ve ever experienced a day ruined by stomach cramps and diarrhea, or if your life is frequently interrupted by unpredictable bowel habits, you’re not alone. These symptoms are not only uncomfortable and socially inconvenient, but they can also signal deeper chronic issues like Irritable Bowel Syndrome (IBS) or inflammatory triggers within the gastrointestinal system.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
Conditions such as constipation and tummy pain, diarrhea abdominal pain, and even stomach cramps constipation often coexist or fluctuate, leaving many patients in a cycle of confusion and mismanagement. For some, the problem is occasional. For others, these symptoms are a recurring reality that severely impacts their quality of life. What complicates the picture even more is that symptoms like bloating and diarrhea, gas and diarrhea, and pain in tummy when pooping can arise from a variety of causes—diet, stress, gut bacteria imbalances, hormonal shifts, and even nervous system dysfunction within the gut wall.
Understanding what causes abdominal cramps and diarrhea, why IBS intestinal gas is so persistent, and how to distinguish an IBS flare from other gastrointestinal disorders is crucial to taking back control. Whether you’re experiencing stomach ache after pooping or wondering what causes belly pain and diarrhea, this article is your in-depth, research-backed guide to decoding your gut distress. We’ll explore the complex relationships between constipation abdominal pain, stomach hurts after pooping, and what an IBS flare up truly feels like. From diagnosis and flare-up triggers to daily symptom management and treatment options, this comprehensive guide is designed to help you better understand your body, reduce fear, and make smarter decisions about your digestive health.
Understanding the Symptom Patterns: When the Gut Sends Alarming Signals
The gastrointestinal tract is a highly sensitive, reactive system designed to digest, absorb, and eliminate food. Yet for many individuals, this process becomes a minefield of discomfort, leading to symptoms like gassy diarrhea, stomach cramps when pooping, or abdominal discomfort diarrhea. Often, these symptoms don’t occur in isolation. Many people find themselves dealing with combinations such as constipation and tummy pain in the morning and sudden stomach ache before pooping in the evening. Such variability points toward functional gastrointestinal disorders like IBS.
Irritable Bowel Syndrome is a chronic condition marked by fluctuating symptoms including bloated stomach and diarrhea, constipation abdominal pain, and pain in intestines and diarrhea. While not considered life-threatening, it can significantly impair quality of life. Unlike infections or structural abnormalities, IBS symptoms are linked to how the brain and gut communicate. Even in the absence of inflammation or visible lesions, patients can experience pain in tummy when pooping or constant diarrhea and gas for days on end.
What makes these symptoms even more alarming is their inconsistency. Some individuals might endure severe intestinal cramps and diarrhea followed by episodes of complete constipation, which only leads to further discomfort and anxiety. This unpredictable pattern makes tracking and managing IBS or similar functional gastrointestinal disorders both frustrating and emotionally exhausting.
What Is an IBS Flare Up? Recognizing the Onset
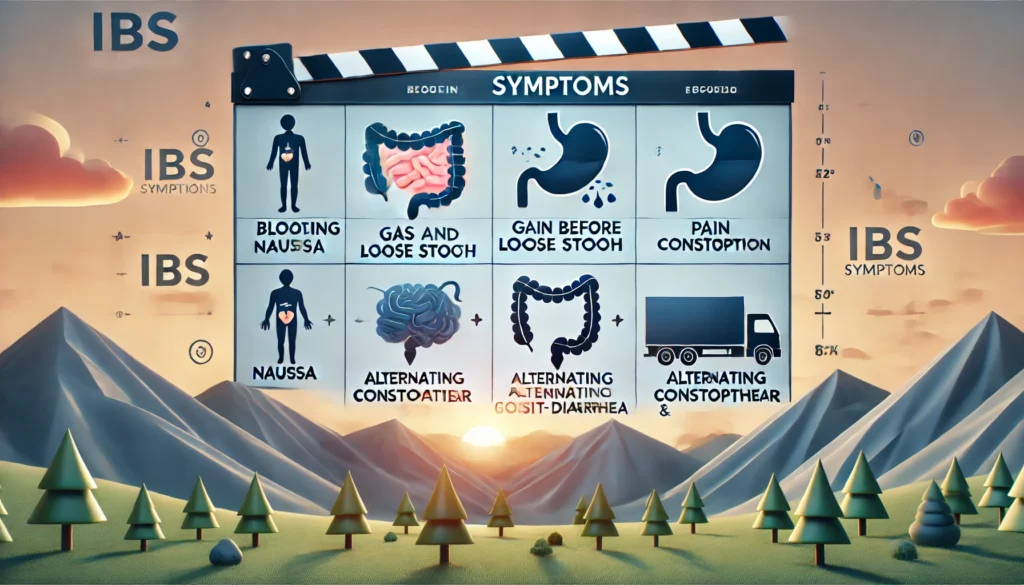
An IBS flare up is a sudden, often severe increase in symptoms like gas and diarrhea, stomach cramps constipation, or abdominal pain constant diarrhea. While every person’s experience is unique, flares are generally characterized by intensified discomfort, urgency to defecate, bloating, and sometimes new or exaggerated sensations such as nausea, vomiting, or fatigue. One of the most commonly asked questions is: does IBS cause nausea or can IBS cause vomiting? The answer is yes—although not all patients experience it, nausea is a documented symptom of IBS and can be exacerbated by diet, stress, or gastrointestinal motility issues.
During a flare, some people report experiencing stomach ache before pooping or feel that their stomach hurts after pooping—signs that the colon is hyper-reactive. IBS intestinal gas, bloating and diarrhea, or severe intestinal cramps and diarrhea can also become more pronounced during this time. Understanding what causes IBS flare ups can help you preemptively manage or even avoid them. Triggers may include dietary choices (high-FODMAP foods), hormonal changes (especially in women), psychological stress, changes in gut microbiota, or even lack of sleep.
Identifying your personal pattern of flare-ups can be life-changing. It allows for targeted interventions such as elimination diets, stress management techniques, or microbiome support that help bring the system back into balance. Recognizing what is an IBS flare up is the first step to reclaiming some control over your digestive health.
IBS and the Complex Relationship Between Constipation and Diarrhea
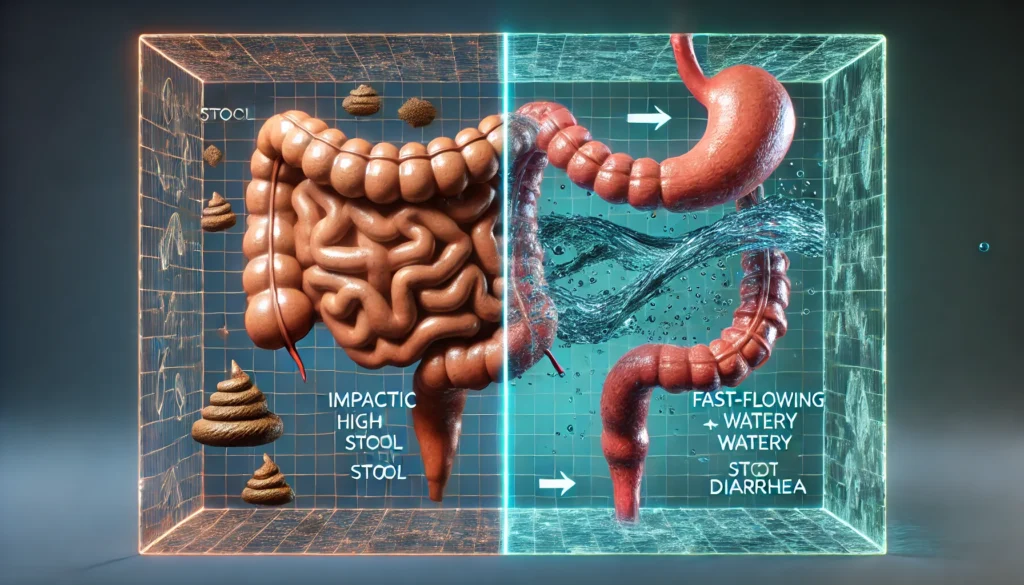
Many people mistakenly believe that IBS presents as either chronic diarrhea or chronic constipation. However, the reality is often a mix. It’s not uncommon to suffer from constipation abdominal pain for days, followed by a sudden shift into diarrhea abdominal pain. This alternation can result in stomach cramps when pooping or an increase in pain in intestines and diarrhea that seems disproportionate to any dietary indiscretion.
IBS is classified into three primary subtypes: IBS-D (diarrhea-predominant), IBS-C (constipation-predominant), and IBS-M (mixed). Those with IBS-M tend to experience constipation and tummy pain followed by bloated stomach and diarrhea, often within the same week—or even the same day. The intestinal walls become hypersensitive, leading to abnormal motility patterns that explain why the stomach hurts after pooping or why gassy diarrhea can persist despite an otherwise healthy diet.
The longer the colon retains stool, the more water it absorbs, leading to harder and more difficult-to-pass stools. When a bowel movement finally happens, it can result in stomach ache after pooping due to muscular contractions or stretching of intestinal walls. Conversely, when stool passes too quickly, as in IBS-D, nutrients and water are not absorbed efficiently, contributing to constant diarrhea and gas, dehydration, and abdominal discomfort diarrhea.
Understanding this cycle helps explain why treatment is never one-size-fits-all. Someone experiencing gas and diarrhea from IBS-D will require a completely different strategy than someone dealing with bloated constipation and stomach ache before pooping in IBS-C. Personalized, flexible treatment approaches are essential.

Diagnosing IBS and Excluding Other Conditions
Given the wide range of symptoms—stomach cramps and diarrhea, constipation and tummy pain, pain in tummy when pooping—it’s easy to misdiagnose IBS or mistake it for other gastrointestinal disorders. This is especially concerning when symptoms escalate and a patient wonders why did my GI symptoms keep getting worse despite making lifestyle changes or following a seemingly appropriate treatment plan.
To diagnose IBS, a thorough medical evaluation is necessary to rule out more serious conditions like Crohn’s disease, ulcerative colitis, celiac disease, or colorectal cancer. Common tests include blood work to check for inflammatory markers, stool tests for infections or parasites, and possibly a colonoscopy or endoscopy. Once other conditions are excluded, IBS is typically diagnosed based on the Rome IV criteria, which focus on recurrent abdominal pain associated with defecation and changes in bowel habits.
A critical part of diagnosis is symptom journaling. Keeping track of when you experience constipation abdominal pain, bloating and diarrhea, or stomach hurts after pooping can help identify patterns and potential triggers. The more detailed your records, the easier it is for a healthcare provider to tailor a treatment plan specific to your body’s needs.
Managing Daily Life with IBS Symptoms
Living with IBS means learning to manage a constellation of symptoms—gas and diarrhea, bloated stomach and diarrhea, pain in intestines and diarrhea—and still maintaining a functioning life. Diet is often the first line of intervention. Many people turn to the low-FODMAP diet, which reduces fermentable carbohydrates that exacerbate IBS intestinal gas and abdominal discomfort diarrhea. While highly effective for some, it’s important that this diet is undertaken with professional guidance, as it is not nutritionally complete for long-term use without reintroduction phases.
Hydration and fiber intake must also be balanced. For individuals dealing with constipation and tummy pain, increasing soluble fiber may ease symptoms. For those with diarrhea abdominal pain, insoluble fiber might worsen issues. Understanding your body’s unique response to different fiber types is crucial. Stress management through meditation, breathwork, yoga, or therapy can also profoundly reduce the frequency and severity of flare-ups.
Medications may include antispasmodics for stomach cramps constipation, anti-diarrheals for constant diarrhea and gas, and laxatives for those experiencing severe blockages. Probiotics and digestive enzymes can also help rebalance gut flora and improve symptoms like bloated stomach and diarrhea or stomach ache before pooping. Because the gut-brain connection is so significant in IBS, some patients also find relief with antidepressants or neuromodulators that alter gut nerve signaling.
Beyond treatment, emotional support is paramount. IBS often comes with a heavy emotional toll—fear of leaving the house, embarrassment in social settings, anxiety about meals. A strong support system, whether through family, therapy, or IBS communities, helps ease the psychological burden and fosters resilience in day-to-day life.
Frequently Asked Questions
1. What causes belly pain and diarrhea at the same time?
Experiencing belly pain and diarrhea simultaneously is often linked to abnormal gut motility, inflammation, or infection. In functional disorders like IBS, this combination can result from the gut’s overreaction to stimuli such as stress, food, or hormonal changes. Bacterial overgrowth or intolerance to fermentable carbs can also cause bloated stomach and diarrhea along with abdominal cramping. If symptoms persist or escalate, it’s important to rule out inflammatory conditions or infections through medical testing.
2. Does IBS cause nausea and vomiting?
Yes, IBS can cause nausea and in rare cases, vomiting. This happens due to delayed gastric emptying, increased intestinal sensitivity, or as a response to pain and bloating. Nausea may also be related to anxiety, which commonly coexists with IBS. Patients often ask, does irritable bowel syndrome cause nausea or can IBS cause vomiting? While these symptoms are less common, they are recognized and should be discussed with a healthcare provider, especially during flare-ups.
3. Why does my stomach ache before pooping?
A stomach ache before pooping often signals intestinal cramping or spasm as the colon tries to move stool. This can occur in IBS due to dysregulated nerve signaling and increased gut sensitivity. The pain is usually relieved by defecation, which supports a diagnosis of IBS. Keeping track of such symptoms can help in identifying patterns that correlate with flare-ups or specific triggers.
4. What causes lots of gas and loose stools?
Excess gas and loose stools are typically caused by rapid fermentation of certain carbohydrates, gut infections, or imbalances in gut bacteria. In IBS, especially IBS-D or IBS-M, this symptom reflects poor nutrient absorption and hyperactive gut motility. Eliminating high-FODMAP foods or working with a registered dietitian to manage microbial balance can significantly improve gas and diarrhea.
5. Why does my stomach hurt after pooping?
If your stomach hurts after pooping, it may be due to residual cramping, incomplete evacuation, or gas trapped in the lower intestine. In IBS, this pain can persist even after bowel movements due to heightened visceral sensitivity. Dehydration, anxiety, or inflammation may also contribute. If the symptom is recurrent, consult your doctor to rule out other gastrointestinal conditions.
6. What triggers abdominal pain and constant diarrhea?
Triggers can include food intolerances, stress, bacterial imbalances, and inflammatory responses. High-fat meals, caffeine, alcohol, or lactose are common culprits. Chronic stress also plays a major role in gut function. Functional issues like IBS can cause ongoing pain and diarrhea without structural damage. Identifying and managing personal triggers through food journals or elimination diets is essential.
7. How do I know if I’m experiencing an IBS flare-up?
Signs of an IBS flare-up include intensified bloating and diarrhea, abdominal cramps, urgent bowel movements, fatigue, and sometimes nausea or mood changes. Many patients also report a sense of fullness or pressure in the abdomen and worsened symptoms after meals. A sudden shift in stool frequency or consistency is a hallmark of flares, especially when coupled with anxiety or poor sleep.
8. Can constipation and diarrhea happen in the same day?
Yes, especially in IBS-M, it’s common for patients to experience alternating bowel patterns. Constipation and tummy pain in the morning may give way to stomach cramps and diarrhea by afternoon. The rapid shift is due to abnormal signaling in the gut’s nervous system, making it harder to regulate movement and water absorption. Keeping a detailed diary can help spot these patterns.
9. Why do my GI symptoms keep getting worse over time?
Worsening GI symptoms can stem from progressive microbial imbalances, unresolved inflammation, increasing sensitivity, or emotional stress. Sometimes, inadequate treatment or ignoring symptoms leads to greater dysfunction. For instance, if someone only treats diarrhea but not the underlying IBS, flare-ups may become more frequent. Comprehensive care addressing gut, diet, stress, and mental health is critical for improvement.
10. Are there long-term consequences of untreated IBS?
While IBS doesn’t cause structural damage like IBD, untreated IBS can severely affect mental health, nutrition, and overall quality of life. Chronic pain, bloating, diarrhea, or constipation may lead to fatigue, social withdrawal, and anxiety. Nutrient deficiencies can arise from avoidance diets or malabsorption. Timely diagnosis and consistent management reduce these risks and support long-term wellness.

Conclusion
Digestive symptoms such as stomach cramps and diarrhea, constipation and tummy pain, or bloated stomach and diarrhea are not just inconvenient—they’re messages from your gut signaling deeper imbalances. Whether triggered by stress, diet, microbial shifts, or neurological sensitivity, these symptoms deserve attention, validation, and informed action. Understanding what causes abdominal cramps and diarrhea, why IBS intestinal gas persists, and how to manage stomach cramps constipation or stomach ache before pooping can transform fear into empowerment.
By identifying personal triggers, tracking flare-up patterns, and seeking medical guidance, you can navigate this complex condition with more clarity and less confusion. Remember, your gut is not just a digestion center—it’s deeply connected to your brain, emotions, and immune system. When symptoms like constant diarrhea and gas or pain in intestines and diarrhea flare up, they require a whole-body approach to healing.
With the right tools, knowledge, and support, it’s entirely possible to live a full, thriving life—even with IBS or chronic digestive issues. Let your journey to gut wellness begin with curiosity, compassion, and a willingness to listen to your body’s wisdom.