Introduction
Leaky gut syndrome, though often misunderstood or overlooked by mainstream medicine, has become a topic of growing interest among functional medicine practitioners, nutritional scientists, and gut health researchers. At its core, leaky gut refers to increased intestinal permeability—a condition in which the lining of the small intestine becomes damaged, allowing undigested food particles, toxins, and bacteria to leak into the bloodstream. This can trigger widespread inflammation and immune system reactions that manifest as digestive distress, chronic fatigue, mood disorders, autoimmune flare-ups, and skin conditions.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
Understanding what is leaky gut and why it occurs is essential to identifying early leaky gut symptoms and preventing long-term damage. From subtle changes in digestion to more systemic symptoms of leaky gut syndrome, this condition has been linked to a surprising range of health concerns, prompting many individuals to search for effective ways to diagnose, treat, and ultimately recover from it. With an increasing number of people turning to gut-focused interventions, questions such as how to heal a leaky gut naturally or how to test for leaky gut at home are more relevant than ever.
As science continues to explore the microbiome, intestinal integrity, and the gut-immune axis, it has become clear that the gut serves as a powerful control center for overall wellness. This article explores leaky gut syndrome in depth, diving into what causes leaky gut, its hallmark signs, diagnostic options, and cutting-edge research on how to fix leaky gut through natural and clinical strategies. For those experiencing digestive challenges, autoimmune issues, or unexplained fatigue, understanding and addressing leaky intestine syndrome may provide the missing piece to full-body healing.
What Is Leaky Gut Syndrome?
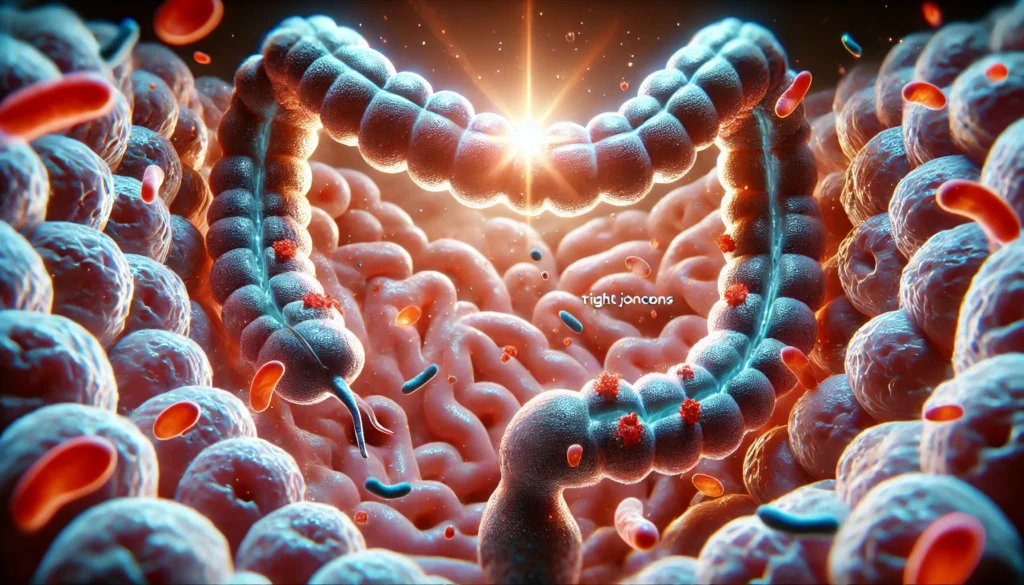
Leaky gut syndrome, also known as leaky bowel disease or leaky gut disorder, is characterized by compromised intestinal barrier function. In a healthy gut, the intestinal wall serves as a tightly regulated gateway, allowing nutrients and water to pass into the bloodstream while keeping harmful substances out. This barrier is maintained by epithelial cells joined by tight junctions, mucus layers, and immune cells that collectively form a semi-permeable shield.
When this barrier becomes disrupted due to stress, poor diet, chronic inflammation, dysbiosis, or environmental toxins, the tight junctions loosen and harmful molecules escape the gut lumen into systemic circulation. This results in an immune response, as the body perceives these foreign particles as threats. Over time, the ongoing immune activation contributes to chronic inflammation, tissue damage, and the development or worsening of autoimmune and inflammatory conditions.
Despite its recognition in functional medicine circles, leaky gut syndrome remains controversial in conventional medical communities. However, recent studies support the concept of increased intestinal permeability as a measurable physiological process linked to diseases such as Crohn’s, celiac disease, irritable bowel syndrome (IBS), rheumatoid arthritis, and even mental health disorders like depression and anxiety.

Common Leaky Gut Symptoms and Clinical Clues
Leaky gut symptoms can vary widely depending on the severity of the barrier dysfunction and the individual’s underlying health conditions. Early symptoms of leaky gut syndrome are often digestive in nature, but over time, systemic manifestations may emerge. Some of the most commonly reported leaky gut symptoms include:
Abdominal bloating, gas, cramps, and irregular bowel movements are hallmark gastrointestinal signs. These symptoms occur due to the disruption of the microbiome and the inflammation that ensues when harmful substances leak through the intestinal wall.
Individuals may also experience food sensitivities and intolerances, particularly to gluten, dairy, soy, or sugar. This happens because the immune system begins attacking proteins from these foods that escape the gut and trigger systemic reactions. Over time, these reactions can increase in intensity and frequency, making dietary choices more limited and frustrating.
Fatigue and brain fog are among the most underappreciated symptoms of leaky gut syndrome. The chronic immune activation can lead to mitochondrial dysfunction, decreased energy production, and impaired cognitive clarity. Many people with leaky gut report feeling persistently tired, forgetful, or mentally sluggish.
Chronic joint pain, skin rashes (like eczema and acne), mood swings, anxiety, and depression may also be indicators of leaky bowel disease. These manifestations highlight the gut-brain and gut-joint axes, where immune messengers and microbial metabolites influence systemic inflammation and neurological function.
When multiple organ systems are affected without a unifying diagnosis, it may be worth considering whether a leaky stomach is playing a role. Recognizing these early and systemic leaky gut symptoms is essential for timely intervention and recovery.
What Causes Leaky Gut Syndrome?
Understanding what causes leaky gut syndrome is critical to preventing and reversing its effects. Several factors have been implicated in increasing intestinal permeability and compromising gut integrity.
A poor diet, particularly one high in sugar, refined carbohydrates, alcohol, artificial additives, and inflammatory fats, is one of the most significant contributors. These foods damage the intestinal lining, disrupt the microbiota, and promote the release of zonulin—a protein known to regulate tight junctions and increase permeability when overexpressed.
Chronic stress also plays a major role in leaky gut disorder. Stress triggers the release of cortisol and other stress hormones, which can decrease mucosal immunity, slow digestion, and impair gut barrier function. Over time, elevated cortisol levels contribute to inflammation and compromise the epithelial lining.
Dysbiosis, or an imbalance of beneficial and harmful gut bacteria, is closely associated with increased intestinal permeability. A lack of microbial diversity and an overgrowth of pathogenic strains can damage the mucosal lining, disrupt immune signaling, and increase leaky gut risk.
Infections, both acute and chronic, can compromise gut integrity. Pathogens such as H. pylori, Candida albicans, Clostridium difficile, and parasites can trigger inflammation and epithelial damage, paving the way for a leaky intestine syndrome.
Medications, including NSAIDs, antibiotics, antacids, and steroids, are known to damage the gut lining and alter microbiota composition. Their overuse has been linked to the development of gastrointestinal disorders and increased permeability.
Finally, genetic predispositions and underlying autoimmune diseases can increase the likelihood of developing leaky gut syndrome. In these cases, a targeted, individualized approach to treatment becomes essential.

How to Diagnose Leaky Gut
Determining how to diagnose leaky gut remains a challenge, as there is no single gold-standard test accepted by all medical practitioners. However, several functional and clinical tests can provide insights into intestinal barrier integrity and immune activation.
One common method involves measuring levels of zonulin, a protein that regulates intestinal permeability. Elevated zonulin levels in blood or stool samples suggest that the tight junctions between intestinal cells are loosening and the barrier is compromised.
Another popular approach is the lactulose-mannitol urine test, which evaluates how well the small intestine absorbs these two sugar molecules. A high ratio of lactulose to mannitol indicates increased permeability.
Antibody-based testing is also available. Some laboratories offer panels that assess immune responses to bacterial endotoxins, lipopolysaccharides (LPS), and other translocated gut proteins. Elevated antibodies can reflect systemic exposure to gut-derived antigens due to barrier dysfunction.
For those wondering how to test for leaky gut at home, several companies now offer at-home testing kits that include zonulin assays or urine sugar permeability tests. While not as comprehensive as lab-based diagnostics, these kits provide a convenient starting point for those exploring symptoms of leaky gut syndrome.
Clinical judgment remains essential. Practitioners often rely on a thorough history, symptom analysis, and exclusion of other gastrointestinal diseases. In many cases, suspected leaky gut is addressed through targeted lifestyle and dietary interventions without formal testing.

Evidence-Based Strategies for How to Heal Leaky Gut
Healing leaky gut syndrome involves restoring the integrity of the intestinal lining, rebalancing the microbiome, and reducing inflammation. Functional medicine often applies the 5R framework: Remove, Replace, Reinoculate, Repair, and Rebalance.
To start, it’s important to remove dietary and lifestyle triggers that contribute to intestinal damage. This includes eliminating processed foods, refined sugars, alcohol, artificial sweeteners, and common allergens such as gluten and dairy. Many practitioners recommend an elimination diet or the autoimmune protocol (AIP) to identify individual food sensitivities.
Replacing essential digestive factors such as stomach acid, bile, and pancreatic enzymes can support digestion and nutrient absorption. This is particularly useful for those with hypochlorhydria or enzyme insufficiencies.
Reinoculation involves replenishing beneficial bacteria through diet and probiotics for leaky gut. Fermented foods like sauerkraut, kefir, and kimchi, along with probiotic supplements, can help restore microbial diversity and compete with pathogenic strains.
Repairing the gut lining is a cornerstone of any leaky gut recovery plan. This is where targeted nutrients and leaky gut supplements come into play. L-glutamine, an amino acid, is widely used for its ability to regenerate intestinal cells. Zinc carnosine, N-acetyl glucosamine, omega-3 fatty acids, vitamin D, and collagen peptides are also supported by research for their roles in mucosal healing and inflammation control.
Rebalancing the body involves managing stress, optimizing sleep, supporting detoxification pathways, and incorporating movement. These lifestyle strategies are critical for reducing cortisol levels, improving immune function, and supporting long-term healing.

The Role of Supplements in Leaky Gut Treatment
The supplement market for leaky gut syndrome has expanded rapidly in recent years. Consumers searching for the best leaky gut supplements or the best supplement for leaky gut syndrome are often met with a dizzying array of options. However, science points to several compounds with consistent evidence of benefit.
L-glutamine is perhaps the most well-researched. This amino acid serves as a primary fuel source for enterocytes, the cells lining the gut wall. Supplementing with glutamine has been shown to reduce permeability and promote intestinal cell regeneration.
Probiotics for leaky gut can help rebalance the microbiome, reduce inflammation, and strengthen the mucosal barrier. Specific strains, such as Lactobacillus rhamnosus GG and Saccharomyces boulardii, have shown promise in reducing intestinal permeability and improving gut-related symptoms.
Other valuable leaky gut syndrome supplements include zinc carnosine, which helps maintain tight junction integrity, and N-acetyl glucosamine, which supports mucus production and epithelial repair. Omega-3 fatty acids are known for their anti-inflammatory effects, while collagen and gelatin provide structural support for connective tissues, including the gut lining.
Botanicals like aloe vera, slippery elm, licorice root (DGL), and marshmallow root offer additional support through their mucilaginous and soothing properties. When used in combination with a therapeutic diet, these supplements can accelerate leaky gut recovery and reduce symptoms significantly.
Before starting any supplementation regimen, it is advisable to work with a healthcare provider familiar with how to treat leaky gut using evidence-based and personalized approaches.
Leaky Gut Recovery: Timeline and Expectations
One of the most frequently asked questions is: how long does it take to heal leaky gut? The answer depends on the individual’s overall health, the severity of their symptoms, their adherence to dietary changes, and the presence of coexisting conditions.
For some, early improvements may be seen in as little as two to four weeks, particularly in digestion and energy levels. More significant or systemic improvements, such as reduced joint pain, clearer skin, and balanced mood, often take three to six months.
Full leaky gut recovery, particularly in individuals with autoimmune disease or long-standing digestive issues, may take six months to a year. Consistency is key—addressing the root causes, using targeted therapies, and maintaining lifestyle changes can make a profound difference.
Monitoring progress through symptom tracking, lab retesting, or periodic assessments can help individuals stay motivated and informed about their healing journey.
While there is no one-size-fits-all solution for how to repair leaky gut, with the right tools and support, recovery is not only possible but empowering.
Frequently Asked Questions
1. How do you know if you have leaky gut?
Identifying leaky gut involves a combination of symptom recognition, personal history, and potentially lab testing. Common signs include digestive discomfort, food sensitivities, brain fog, fatigue, skin issues, and autoimmune flares. If multiple symptoms overlap and improve with dietary and lifestyle interventions, leaky gut may be the underlying cause. Functional medicine practitioners may use zonulin tests or permeability assessments for further clarity.
2. What causes leaky gut in the first place?
Leaky gut can be caused by dietary factors, chronic stress, dysbiosis, infections, medication use, and environmental toxins. Processed foods, sugar, alcohol, antibiotics, and nonsteroidal anti-inflammatory drugs are common culprits. Genetics and autoimmune diseases can also predispose someone to developing intestinal permeability.
3. How to heal a leaky gut naturally?
Natural healing strategies focus on removing inflammatory triggers, repairing the gut lining with nutrients like L-glutamine and collagen, restoring microbial balance with probiotics and prebiotics, and reducing stress. A whole-foods diet, rich in fiber, fermented foods, and anti-inflammatory nutrients, forms the foundation of natural recovery.
4. Are there at-home tests for leaky gut?
Yes, at-home test kits are available from several companies. These may include zonulin stool tests, urine sugar absorption tests, and finger-prick blood spot tests for gut-derived antibodies. While not diagnostic on their own, these tests offer insights into gut barrier status and can guide further investigation or treatment.
5. What is the best supplement for leaky gut syndrome?
L-glutamine is often considered the best supplement for leaky gut due to its direct role in intestinal cell repair. Zinc carnosine, N-acetyl glucosamine, collagen, and targeted probiotics are also highly effective. The best leaky gut supplements often combine several of these nutrients in a synergistic formula.
6. How long does it take to fix leaky gut?
Healing timelines vary, but many people begin to see symptom improvements within four to six weeks of implementing changes. Deeper, long-term healing can take several months. Factors such as stress management, dietary adherence, and chronic disease status will influence the duration of recovery.
7. Can probiotics help leaky gut?
Absolutely. Probiotics for leaky gut can enhance gut barrier function, modulate immune responses, and crowd out pathogenic bacteria. Specific strains like Lactobacillus and Bifidobacterium have been shown to reduce intestinal permeability and support microbial diversity. Probiotics should be introduced gradually and tailored to the individual’s needs.
8. How is leaky gut diagnosed clinically?
There is no universally accepted clinical diagnosis, but tests like zonulin assays, lactulose-mannitol tests, and gut antibody panels are used in functional medicine. Diagnosis often involves ruling out other gastrointestinal diseases and identifying symptoms consistent with increased permeability. A personalized assessment is essential.
9. Is leaky gut a real condition?
Yes. While the term “leaky gut syndrome” is not commonly used in conventional medicine, the concept of increased intestinal permeability is well-documented in scientific literature. It has been linked to celiac disease, IBD, IBS, diabetes, and other inflammatory conditions. Growing evidence supports its role in systemic illness and the importance of gut barrier function.
10. What is the best diet for leaky gut?
A diet focused on whole, unprocessed foods, anti-inflammatory ingredients, and low-allergen content is ideal. The leaky gut diet often eliminates gluten, dairy, refined sugar, and additives while emphasizing vegetables, bone broth, healthy fats, lean proteins, and fermented foods. Tailoring the diet to the individual’s sensitivities enhances effectiveness.

Conclusion
Leaky gut syndrome is a multifaceted condition with widespread implications for health and wellness. Recognizing leaky gut symptoms early, understanding what causes leaky gut, and implementing strategic interventions can prevent long-term complications and support recovery. Whether someone is newly exploring how to diagnose leaky gut, searching for the best leaky gut supplements, or committed to discovering how to cure leaky gut naturally, the evidence-based strategies explored here offer a comprehensive roadmap to healing.
While leaky gut disorder may not yet be fully embraced by conventional medicine, the science supporting intestinal permeability and its systemic impact is rapidly expanding. As research continues to bridge gaps between functional and allopathic perspectives, more people can access the tools they need for vibrant gut health.
Through diet, supplements, lifestyle adjustments, and professional guidance, repairing the intestinal lining is within reach. Healing the gut truly heals the whole body—bringing clarity, energy, immunity, and resilience to those willing to take the journey.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
How long does it take to heal leaky gut?
Leaky gut: What is it, and what does it mean for you?
Leaky Gut Syndrome: Symptoms, Causes, Diagnosis, and Treatment



