Introduction
Irritable Bowel Syndrome, commonly referred to as IBS, is a functional gastrointestinal disorder that affects millions of people globally, yet remains frustratingly complex to diagnose, treat, and fully understand. Within the spectrum of IBS subtypes, IBS-C—or irritable bowel syndrome with constipation—is one of the most commonly reported and also one of the most uncomfortable. It’s characterized by abdominal pain, bloating, and infrequent, difficult bowel movements. But its symptoms don’t stop there. Many individuals experience overlapping health concerns that impact daily life, emotional well-being, and long-term quality of health.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
Despite its prevalence, many patients struggle for years without a clear answer, often left wondering, how is IBS diagnosed or even is IBS a dangerous disease. This confusion stems in part from the syndrome’s broad presentation. IBS symptoms vary significantly from person to person, and what causes an IBS flare-up in one individual may be completely benign in another. This makes both diagnosis and treatment a nuanced process—one that requires careful consideration of physical, emotional, dietary, and sometimes even hormonal factors.
In particular, IBS symptoms in women can be more severe and cyclical due to hormonal fluctuations. The experience of stomach discomfort after a bowel movement, gas retention, bloating, or IBS pain that radiates across the abdomen can all indicate IBS-C, especially when constipation is chronic. Many people ask: Can IBS be cured? Is irritable bowel syndrome curable? Or perhaps most urgently: How to cure IBS permanently? The answers are layered, involving dietary adjustments, medication, lifestyle interventions, and sometimes gut-focused psychotherapies.
This article is a deep dive into the science of IBS, with a focus on IBS-C. We will explore its symptoms, potential causes, diagnostic methods, conventional and alternative treatments, and the latest research on whether IBS is curable. We will also consider how long it takes to get diagnosed with IBS, how to differentiate between subtypes like IBS-D and IBS-C, and what to do when your stomach aches after a bowel movement or you’re experiencing persistent IBS constipation. Whether you’re newly diagnosed, seeking better solutions, or searching for clarity about whether IBS can go away, this is your definitive, expert-level guide.
Understanding IBS-C: What It Is and Why It Matters
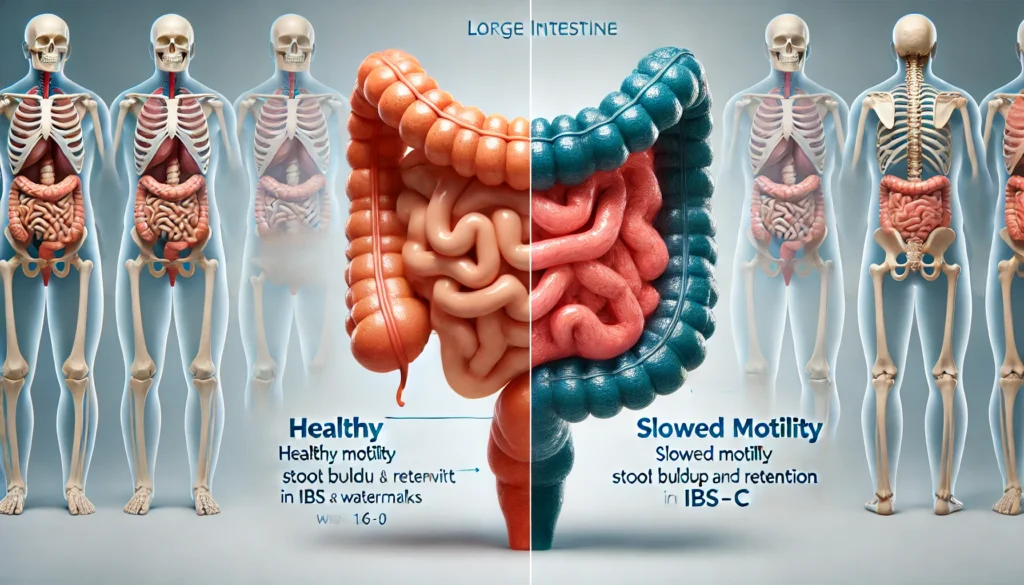
IBS-C stands for irritable bowel syndrome with constipation. It is a subtype of IBS where constipation dominates the symptom profile. People with IBS-C frequently report hard or lumpy stools, infrequent bowel movements, and a sense of incomplete evacuation. This subtype is not simply a mild inconvenience. It can significantly impact a person’s physical comfort and emotional stability, especially when symptoms are chronic and unpredictable.
Unlike temporary constipation caused by diet or dehydration, IBS constipation is part of a broader functional disorder. The motility of the gut is often impaired, meaning that the muscles of the intestine do not move food and waste through efficiently. Moreover, the gut-brain axis—an intricate communication system between the digestive tract and the central nervous system—often plays a key role in triggering or exacerbating symptoms. Stress, anxiety, and hormonal shifts can all disrupt this axis and lead to flare-ups.
The phrase IBS symptoms often encompasses more than just digestive distress. Individuals with IBS-C may also experience fatigue, brain fog, back pain, bloating, and urinary issues. These symptoms can fluctuate in intensity and frequency, making the disorder difficult to predict and manage. For many, IBS flare-up symptoms are triggered by specific foods, emotional stress, hormonal changes (particularly for women), or even travel and sleep disruption.

How Is IBS Diagnosed?
One of the most frustrating aspects of irritable bowel syndrome is the process of diagnosis. Unlike conditions that are easily identified through a blood test or imaging scan, IBS is diagnosed primarily through clinical criteria and the exclusion of other conditions. The Rome IV criteria, a standardized diagnostic framework, is commonly used. According to this guideline, a person must have recurrent abdominal pain at least one day per week in the last three months, associated with at least two of the following: pain related to defecation, a change in stool frequency, or a change in stool form.
Doctors may also order tests to rule out other gastrointestinal conditions, such as celiac disease, inflammatory bowel disease (IBD), colon cancer, and infections. This may involve blood tests, stool analysis, colonoscopy, or imaging studies. Understanding how IBS is diagnosed is essential because it’s often a diagnosis of exclusion—meaning it’s only confirmed after other more serious conditions are ruled out.
It’s not uncommon for patients to spend years navigating various specialists, experiencing medical gaslighting, or being told their symptoms are “in their head.” This makes the diagnosis process not only medical but also deeply emotional. Understanding the legitimacy and science behind IBS-C helps counter the stigma and encourages appropriate care. People often wonder how long to get diagnosed with IBS, and the truth is that delays are common. Persistent advocacy, informed questions, and a knowledgeable gastroenterologist can accelerate the process.
What Causes IBS-C? Exploring Root Factors
The precise cause of irritable bowel syndrome is still not fully understood, but most researchers agree that it is multifactorial. This means that IBS-C likely arises from a combination of factors—gut motility dysfunction, altered pain perception, microbial imbalance, inflammation, and brain-gut communication errors.
Diet is a well-established trigger. High-FODMAP foods, which are fermentable sugars found in various fruits, vegetables, and grains, are known to exacerbate symptoms in many people with IBS. For those with IBS-C, insoluble fiber or lack of water may further contribute to stomach discomfort after a bowel movement. Identifying personal food triggers is often essential in symptom control.
Gut microbiota is another major player. People with IBS often show reduced diversity of gut bacteria, including lower levels of beneficial strains. This dysbiosis may affect the fermentation of food in the intestines, leading to gas, bloating, and irregular stool formation. The question can IBS cause sickness becomes especially relevant when microbial imbalance also impairs nutrient absorption or contributes to systemic inflammation.
Stress is not merely a trigger—it can be a cause. The enteric nervous system, sometimes called the “second brain,” manages digestion and is deeply intertwined with emotional regulation. Prolonged stress alters gut motility, enzyme secretion, and microbiota health, often leading to exacerbated IBS flare-up symptoms. Hormonal fluctuations—especially in women—also play a role. Estrogen and progesterone influence gastrointestinal function, which may explain why IBS symptoms in women often worsen around menstruation.

Recognizing Symptoms: IBS-C and Beyond
The hallmark IBS C symptoms include hard or lumpy stools, infrequent bowel movements (typically fewer than three per week), straining during defecation, abdominal pain, and bloating. However, the symptom picture is often much broader. Some individuals report stomach ache after bowel movement that persists for hours. Others feel a constant fullness or heaviness in the lower abdomen.
In women, hormonal cycles can intensify symptoms. IBS symptoms in women often present alongside menstrual cramps or are mistaken for gynecological issues. Fluctuating estrogen levels can influence gut motility, making constipation more likely in the luteal phase of the cycle.
Can I get IBS pain on one side of the abdomen? The answer is yes. IBS pain is often cramping in nature and may localize to either the left or right lower quadrant. It’s important to distinguish this from other conditions such as appendicitis, diverticulitis, or ovarian cysts.
Some people also wonder can IBS be cured or treated when symptoms are cyclical or change over time. In some cases, people report a gradual shift from IBS-C to IBS-D or a more mixed form. This evolution underscores the complexity of the syndrome and the importance of individualized treatment.
Conventional Treatment Approaches for IBS-C
When people seek IBS medication or irritable bowel syndrome medication, they’re often prescribed antispasmodics, laxatives, or fiber supplements. In the United States, FDA-approved drugs for IBS-C include linaclotide (Linzess), plecanatide (Trulance), and lubiprostone (Amitiza). These medications work by increasing intestinal fluid and motility, making it easier to pass stool and reducing pain signals.
Over-the-counter remedies include polyethylene glycol (PEG), psyllium husk, or magnesium-based laxatives. While helpful in relieving IBS constipation, they may not address the full symptom spectrum, especially when stress and diet are major factors.
Dietary interventions are also foundational. The low-FODMAP diet, developed by Monash University, involves restricting certain fermentable carbohydrates to reduce bloating and discomfort. After a short elimination phase, foods are reintroduced systematically to identify specific triggers.
Some patients benefit from psychotherapy. Cognitive-behavioral therapy (CBT), gut-directed hypnotherapy, and mindfulness-based stress reduction (MBSR) have shown strong efficacy in IBS studies. These approaches address the psychological components that influence gut function, supporting the notion that IBS can be cured or treated when approached holistically.

Alternative and Functional Medicine Strategies
For those exploring how to cure IBS permanently, functional medicine offers some promising strategies. These often include comprehensive stool testing, food sensitivity screening, SIBO breath tests, and in-depth hormonal assessments. Treatment protocols may involve antimicrobials for bacterial overgrowth, probiotics, anti-inflammatory supplements, and targeted dietary changes.
Acupuncture has shown some promise in modulating gut motility and reducing pain. Herbal remedies like peppermint oil, fennel seed, and ginger are also commonly used in integrative approaches.
While there’s no universal cure, combining these approaches can yield long-term remission. Many practitioners believe that IBS can go away—or at least be controlled to the point of non-disruption—if its root causes are effectively identified and treated.
Frequently Asked Questions
1. What are the most common IBS-C symptoms?
IBS-C symptoms typically include infrequent bowel movements, hard or lumpy stools, abdominal pain, bloating, and a sensation of incomplete evacuation. Additional symptoms such as gas, fatigue, and stomach discomfort after a bowel movement are also common. These symptoms can vary in intensity and often worsen with stress or dietary changes. Many women report worsened symptoms during hormonal shifts or around menstruation, adding complexity to their experience.
2. How is IBS different from IBD?
While both IBS and inflammatory bowel disease (IBD) affect the gastrointestinal system, they are fundamentally different. IBS is a functional disorder—meaning no visible inflammation or tissue damage is usually present. IBD, on the other hand, involves chronic inflammation that can cause ulcers, strictures, and other damage to the digestive tract. Unlike IBD, IBS rarely leads to long-term physical complications, though its quality-of-life impact can be profound.
3. Can IBS-C lead to serious complications?
IBS-C itself is not considered life-threatening and does not cause permanent damage to the digestive tract. However, the chronic nature of symptoms can lead to secondary issues such as hemorrhoids from straining, nutritional deficiencies due to dietary restrictions, or emotional stress and depression. This is why treatment is essential—not to prevent death, but to preserve quality of life and psychological health.
4. What’s the best medication for IBS-C?
The best IBS medication depends on the severity of symptoms and the individual’s response to different treatments. FDA-approved drugs like Linzess, Amitiza, and Trulance are often effective for those with severe IBS constipation. However, many people manage symptoms with dietary fiber, lifestyle changes, probiotics, and stress reduction. A combination of approaches tends to offer the most sustained relief.
5. How long does it take to get diagnosed with IBS?
Many patients report delays in diagnosis due to the overlap of symptoms with other gastrointestinal conditions. On average, it can take months or even years. Doctors often perform tests to rule out infections, IBD, and celiac disease before diagnosing IBS. Familiarity with the Rome IV criteria can help speed up the process and improve communication between patient and provider.
6. Is IBS curable or just manageable?
There is no universally recognized “cure” for IBS, but many people achieve long-term remission through personalized care. A combination of dietary modification, stress reduction, gut healing protocols, and targeted medication can lead to a near-symptom-free life. In this sense, while IBS may not be curable in the traditional sense, it is absolutely treatable—and for many, fully manageable.
7. Can IBS symptoms shift over time?
Yes, many patients experience a shift between subtypes of IBS over time. Someone with IBS-C symptoms today may develop diarrhea-predominant symptoms later, leading to a classification of IBS-M (mixed). These shifts can be triggered by infections, medication, hormonal changes, or dietary disruptions, and they often complicate long-term treatment planning.
8. Are IBS symptoms different in women?
IBS symptoms in women often vary in intensity based on the menstrual cycle. Hormonal fluctuations affect gut motility and visceral sensitivity, leading to more pronounced symptoms in the days before menstruation. Additionally, women are more likely to report nausea and upper abdominal discomfort compared to men, who tend to experience more bloating and lower abdominal pain.
9. Can IBS be triggered by emotional stress?
Absolutely. The gut-brain axis plays a significant role in IBS flare-up symptoms. Emotional stress can alter gut motility, increase visceral hypersensitivity, and impact microbiota balance. Many patients notice that stressful life events correlate closely with worsening symptoms. Psychological support and stress-reducing practices are therefore key components of effective IBS treatment.
10. What can I do to stop IBS symptoms quickly?
To stop IBS symptoms in the short term, it’s helpful to rest, hydrate, use heat therapy for cramping, and stick to easily digestible foods. Peppermint oil capsules can offer quick relief for spasms. Long-term strategies include the low-FODMAP diet, fiber regulation, stress management, and possibly medication. Fast relief is possible, but consistency in treatment is what offers lasting control.

Conclusion
IBS-C is more than just constipation—it is a complex, chronic condition that affects both the body and mind. It involves a delicate interplay between diet, stress, hormones, and gut microbiota, making its management both a science and an art. While there may not yet be a universal cure, irritable bowel syndrome can be treated effectively with a personalized and integrative approach that addresses the root causes, not just the symptoms.
From FDA-approved medications and low-FODMAP diets to cognitive therapies and functional medicine protocols, the tools for healing are abundant and continually evolving. The most important step is seeking knowledgeable care, understanding your triggers, and being proactive in managing your symptoms. Whether you’re dealing with IBS-C symptoms, wondering how to cure IBS permanently, or exploring whether IBS can go away, remember that progress is possible—and relief is within reach.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine



