Breastfeeding is widely recognized as a critical foundation for an infant’s nutrition, immunity, and emotional development. For parents seeking clarity on how long should infants breastfeed to achieve healthy growth milestones, the guidance can seem both overwhelming and sometimes contradictory. Nonetheless, understanding the nuances of infant and toddler feeding patterns can empower caregivers to make informed, evidence-based decisions. Experts in pediatric health and nutrition agree that breastfeeding is not just about nourishment—it is a dynamic process that evolves in response to a baby’s developmental needs. In this comprehensive guide, we will explore the physiological, psychological, and social dimensions of breastfeeding duration, examine how breastfeeding impacts infant development, and offer practical strategies to support families on this critical journey.
You may also like: Essential Milestones in Baby Led Weaning: A Proven Guide to Nurturing Healthy Eating Habits
Why Breastfeeding Matters in Early Development
Breast milk is uniquely tailored to meet the evolving nutritional requirements of infants, especially during the critical first months of life. Its composition shifts daily—and even during individual feedings—to match the child’s growth and immune system demands. In the earliest days postpartum, the mother produces colostrum, a thick, golden substance rich in antibodies and immune-boosting properties. This transitional milk gradually matures into a balance of proteins, fats, carbohydrates, vitamins, and enzymes that support healthy brain development and gastrointestinal maturity.
Research consistently shows that exclusive breastfeeding for at least the first six months reduces the risk of respiratory infections, gastrointestinal illnesses, and sudden infant death syndrome (SIDS). It also contributes significantly to the development of a stable gut microbiome, which is essential for long-term immune regulation. Beyond physical health, breastfeeding nurtures the mother-infant bond, regulates infant stress responses, and contributes to secure attachment—all foundational aspects of emotional and social development. Understanding how long should you breastfeed to optimize these benefits requires a nuanced look at developmental stages and evolving nutritional needs.
The Recommended Duration: Understanding the Global Consensus
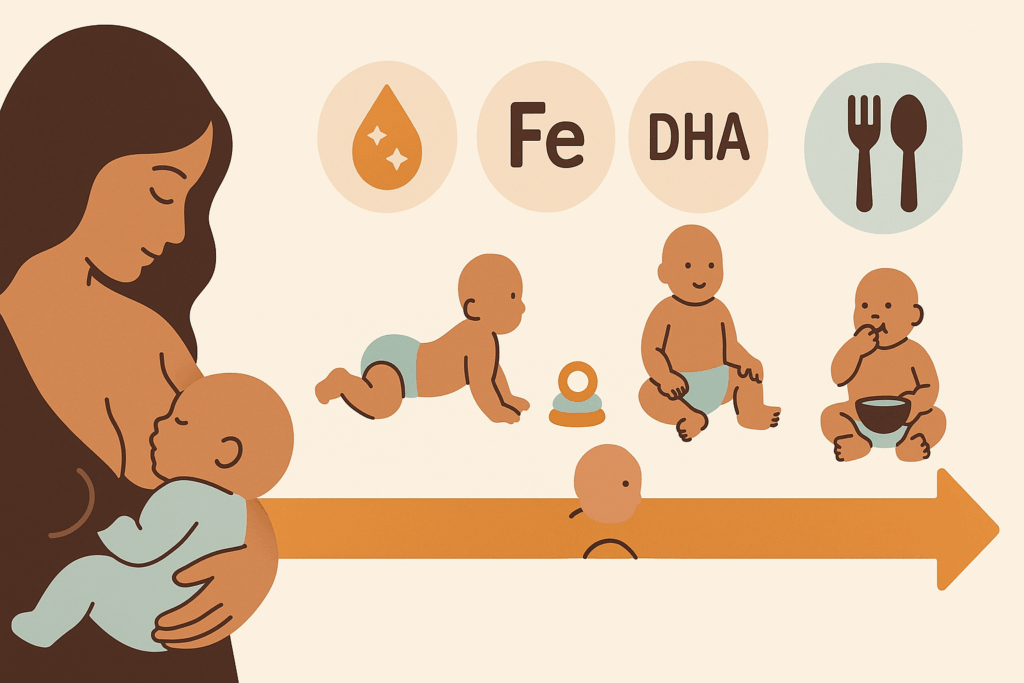
Health organizations around the world, including the World Health Organization (WHO) and the American Academy of Pediatrics (AAP), recommend exclusive breastfeeding for the first six months of life, followed by continued breastfeeding along with complementary foods for up to two years or beyond. This recommendation is based on a wealth of evidence showing that long-term breastfeeding continues to provide essential nutrients and immunological protection well past infancy.
For example, studies indicate that the nutritional value of breast milk remains significant into the toddler years, with elevated levels of immunoglobulins, enzymes, and fatty acids. These components are especially important as toddlers explore diverse environments and face increased exposure to pathogens. Parents often wonder how long can you breastfeed without diminishing returns, and the research affirms that benefits extend well into the second year and even longer. While cultural attitudes and practical constraints may affect duration, aligning with these global standards supports optimal health outcomes.
How Long Should Infants Breastfeed for Immune and Brain Development
Breastfeeding plays a crucial role in the formation of the infant’s immune system and brain architecture. The presence of bioactive components—such as lactoferrin, oligosaccharides, and immunoglobulin A—helps protect against infections and modulates inflammatory responses. These benefits are cumulative, meaning that the longer an infant breastfeeds, the stronger and more resilient their immune system tends to become.
Additionally, human milk provides essential fatty acids like DHA (docosahexaenoic acid), which are critical for the development of the central nervous system. During the first 1,000 days of life—from conception to age two—the brain undergoes rapid growth, forming neural connections at an astounding rate. Breastfeeding during this window supports cognitive functions, including memory, language acquisition, and attention regulation. These outcomes suggest that the question of how long should infants breastfeed is not just about nutrition, but also about supporting complex developmental processes that shape long-term wellbeing.
How Long Should a Newborn Feed for in the Early Weeks
The frequency and duration of feeding sessions can vary widely during the newborn period, but there are general guidelines that can help caregivers understand what to expect. Newborns typically feed every two to three hours around the clock in the first few weeks. Each feeding session may last anywhere from 10 to 45 minutes, depending on the baby’s age, alertness, latch quality, and milk flow.
Understanding how long should a newborn feed for is essential for ensuring adequate weight gain and hydration. Frequent feedings stimulate milk production and ensure that the baby receives both the foremilk, which quenches thirst, and the hindmilk, which is richer in fat and calories. These early patterns may shift gradually as the baby grows and becomes more efficient at nursing, but monitoring diaper output, weight gain, and overall alertness are crucial metrics for evaluating feeding effectiveness. Newborn feeding patterns can be demanding, but they serve as the physiological groundwork for a thriving infant.
When Do Infants Stop Eating Every 3 Hours?
As infants grow and develop, their feeding schedules typically evolve. Most babies begin to extend the time between feedings around six to eight weeks of age. By three to four months, some infants may go longer stretches—up to four or five hours—between daytime feeds, particularly if they are nursing more efficiently or receiving expressed breast milk from a bottle. However, it’s important to recognize that feeding patterns are not one-size-fits-all and are influenced by factors such as growth spurts, developmental leaps, and individual temperament.
Parents often ask when do infants stop eating every 3 hours as they anticipate more predictable routines. While many babies consolidate feedings by four to six months, others may maintain frequent nursing sessions due to teething, illness, or changes in their environment. Breastfeeding on demand, rather than on a rigid schedule, is still encouraged to ensure that both nutritional and emotional needs are met. The gradual spacing of feeds is a natural progression and a sign of maturing circadian rhythms and metabolic regulation.
How Long Should You Breastfeed for Healthy Growth Trajectories
Assessing growth involves monitoring both weight gain and developmental milestones. Breastfed infants typically grow rapidly in the first three months and then exhibit a more gradual weight gain trajectory compared to formula-fed peers. This pattern is normal and should not be a cause for concern if the baby is meeting developmental benchmarks and appears alert, active, and content.
Pediatricians use growth charts provided by the WHO to track these metrics, and breastfeeding duration plays a direct role in supporting sustained, balanced growth. So how long should you breastfeed to ensure healthy development? While six months of exclusive breastfeeding establishes a solid foundation, continued nursing through the first and second year complements solid food intake and supplies vital nutrients such as vitamin A, calcium, and long-chain polyunsaturated fatty acids. Prolonged breastfeeding also supports oral-motor development, particularly when bottle-feeding is minimized, which has downstream effects on speech, chewing, and jaw strength.

How Long Do Babies Breastfeed When Starting Solids?
The introduction of solid foods—typically around six months—does not signal an abrupt end to breastfeeding. Rather, it marks the beginning of a complementary feeding period in which breast milk remains a primary source of nutrition while offering infants new textures, flavors, and nutrient sources. Parents often ask how long do babies breastfeed once solids are introduced, and the answer is generally “as long as they desire.” Breastfeeding frequency may decrease slightly over time but remains essential for filling nutritional gaps and reinforcing immune defenses.
During this transitional phase, breast milk provides critical nutrients such as zinc and iron, which are more bioavailable in human milk than in most complementary foods. Continued nursing also provides comfort during the emotional and sensory challenges of trying new foods. It is common for babies to breastfeed before or after meals, depending on their cues and hunger levels. Allowing the infant to self-regulate ensures a positive feeding experience and encourages healthy habits for the future.

The Social and Cultural Influences on Breastfeeding Duration
Despite medical recommendations, the actual duration of breastfeeding varies significantly across different societies, often influenced by cultural norms, workplace policies, and familial expectations. In some communities, breastfeeding into the toddler years is normalized and supported, while in others, early weaning is more common due to social stigma or logistical challenges. These differences highlight the need for public health messaging that respects cultural context while promoting scientifically backed practices.
Mothers navigating how long breast feed recommendations can experience both internal and external pressures. Support from partners, employers, and healthcare providers plays a critical role in enabling sustained breastfeeding. Workplace accommodations—such as lactation breaks and private spaces for pumping—are instrumental in maintaining milk supply for mothers returning to work. Broader societal acceptance, informed by education and advocacy, fosters an environment in which extended breastfeeding is seen as a positive and achievable goal.
How Long Can You Breastfeed Without Supplementing?
One of the most common concerns among new mothers is whether exclusive breastfeeding will continue to meet their baby’s nutritional needs beyond the early months. Evidence shows that breast milk alone is sufficient for most healthy, full-term infants for the first six months. However, after this period, complementary foods are necessary to meet increased energy and micronutrient demands, particularly iron and zinc. Even with the introduction of solids, breast milk remains a valuable source of macronutrients and protective factors.
Understanding how long can you breastfeed without supplementing involves monitoring both the infant’s growth and the mother’s milk supply. Many women can successfully breastfeed well beyond the first year with minimal supplementation, provided that complementary feeding is well-balanced. Mothers of preterm or low-birthweight infants may need additional guidance to ensure adequate intake. Ultimately, frequent nursing, skin-to-skin contact, and responsive feeding are the most reliable strategies for supporting long-term lactation.
When Can You Stop Feeding Baby Every 3 Hours: Sleep, Routine, and Development
Infants typically begin to develop more consistent sleep patterns and feeding intervals by the time they are three to six months old. This is also when parents begin to wonder when can you stop feeding baby every 3 hours and whether longer stretches of sleep are developmentally appropriate. Sleep consolidation is a gradual process, and while some infants can sleep for six or more hours at night by four months, others continue to wake for comfort or hunger.
Reducing nighttime feedings should always be baby-led. Attempts to enforce rigid schedules or sleep training before a baby is developmentally ready can disrupt feeding patterns and lead to reduced milk supply. That said, recognizing signs of readiness—such as increased daytime intake, longer sleep cycles, and consistent weight gain—can help guide parents in making adjustments that support both infant health and caregiver well-being. Responsive parenting remains the gold standard for managing these transitions.
Addressing Common Breastfeeding Challenges That Affect Duration
Breastfeeding is not without its challenges, and many mothers face obstacles that influence how long they are able or willing to continue. Issues such as latch difficulties, nipple pain, low milk supply, and infant reflux can make the experience stressful. However, with timely intervention and expert support, many of these challenges are manageable and need not result in premature weaning.
Access to lactation consultants, peer support groups, and pediatric guidance can significantly improve outcomes. In cases where breastfeeding must be paused due to medical conditions or maternal absence, expressed milk or donor milk are viable alternatives. Understanding that flexibility and adaptation are part of the journey helps reduce guilt and empowers mothers to make choices that align with their circumstances while still honoring the goal of optimal infant nutrition.
Extending Breastfeeding into Toddlerhood: Myths and Realities
Breastfeeding beyond the first year is sometimes met with skepticism or misinformation, yet it is both biologically normal and nutritionally beneficial. Toddlers continue to derive calories, healthy fats, and immune support from breast milk, especially during illnesses when appetite for solid foods may wane. Moreover, nursing can be a valuable tool for emotional regulation and maintaining connection during developmental transitions such as weaning from the bottle or starting daycare.
Common myths—such as breast milk losing its nutritional value after one year or extended nursing causing dependency—are not supported by scientific evidence. Instead, long-term breastfeeding aligns with the natural weaning age observed in many cultures, which ranges from two to four years. Dispelling these misconceptions enables parents to follow their instincts and their child’s cues without undue influence from cultural taboos.
How Long Should Infants Breastfeed in Special Situations
Certain medical or developmental conditions may influence breastfeeding duration and approach. For example, infants born prematurely often have different nutritional needs and may require fortification of breast milk or supplemental feeding techniques. Similarly, babies with cleft palate, neurological impairments, or metabolic disorders may need modified breastfeeding strategies to ensure safety and adequate intake.
In such cases, lactation support becomes even more essential. Expressed milk, supplemental nursing systems, and specialized feeding plans can all help support a breastfeeding relationship despite physical challenges. Parents navigating these situations deserve tailored guidance that respects their unique circumstances and goals. Ultimately, the question of how long should infants breastfeed in these scenarios is answered not by rigid timelines but by individualized care plans that prioritize both nutritional adequacy and family dynamics.
Frequently Asked Questions: How Long Should Infants Breastfeed for Healthy Development and Growth
How long should infants breastfeed in families with food insecurity or limited access to healthcare?
In situations where families face food insecurity or have limited access to reliable healthcare, extended breastfeeding offers a critical line of nutritional and immunological defense. Breast milk requires no financial investment and provides safe, uncontaminated sustenance even in areas with compromised water or food supplies. In such contexts, determining how long should infants breastfeed becomes a matter not only of nutrition but of survival and resilience. Infants who breastfeed for extended periods—especially past the first year—are more likely to maintain adequate nutrition during shortages and may be less susceptible to common infections that thrive in resource-limited environments. Healthcare professionals in these settings often advocate breastfeeding well into toddlerhood as a protective measure against the compounded risks of malnutrition and inadequate medical care.
What psychological benefits are linked to extended breastfeeding?
Extended breastfeeding fosters a deepened emotional connection between the infant and caregiver, which supports secure attachment and healthy social-emotional development. Research suggests that babies who breastfeed beyond infancy often display higher levels of emotional regulation, social responsiveness, and resilience to stress. These outcomes may be attributed to the calming neurochemical responses activated during nursing, including increased oxytocin and reduced cortisol levels. While the conversation often centers on how long should a newborn feed for, the long-term psychological effects of sustained nursing are equally worthy of attention. In a fast-paced world where early childhood stressors are increasing, extended breastfeeding can act as a stabilizing force during transitions such as starting daycare or experiencing household changes.
How long do babies breastfeed when navigating developmental milestones such as teething or sleep regressions?
Developmental transitions like teething, learning to crawl, or undergoing sleep regressions often coincide with temporary increases in breastfeeding frequency and duration. Babies may return to nursing more often for comfort, even if they had begun to space out feedings. These shifts highlight that how long do babies breastfeed is not solely dictated by nutritional needs but also by their desire for soothing and reassurance. During these phases, breast milk continues to provide not only sustenance but also analgesic properties that can ease physical discomfort. Rather than seeing these regressions as setbacks, parents can view them as biologically normal responses where breastfeeding serves as an adaptive tool for navigating change.
How long can you breastfeed while managing work and travel demands?
Many parents are surprised to learn how long can you breastfeed even when navigating the logistical challenges of employment, commuting, or frequent travel. With the right support systems—such as access to lactation rooms, portable pumps, and storage solutions—many individuals continue breastfeeding well beyond the first year while working full-time. Some families adopt a hybrid approach, nursing in the morning and evening while relying on pumped milk during the day. Others implement nursing vacations or increased skin-to-skin time on weekends to sustain supply and connection. Continued lactation in these circumstances often requires coordination, but it proves both feasible and rewarding for families committed to the long-term benefits of breastfeeding.
When can you stop feeding baby every 3 hours at night and still maintain milk supply?
As babies mature, many naturally begin to consolidate nighttime sleep and require fewer feedings. For most infants, this transition begins around three to six months, though it can vary. Understanding when can you stop feeding baby every 3 hours requires observing patterns of growth, sleep, and feeding efficiency. If the baby is nursing well during the day, gaining weight, and producing sufficient wet diapers, occasional longer stretches at night are usually safe. To maintain milk supply during this transition, some caregivers choose to pump once overnight or increase frequency during daytime feeds. This adjustment period often requires flexibility and reassurance that every baby follows a slightly different timeline.
How long should a newborn feed for during growth spurts or illness?
Growth spurts—often occurring around 7–10 days, three weeks, six weeks, and three months—typically trigger increased nursing duration and frequency. During these phases, how long should a newborn feed for may expand significantly as the infant signals a temporary spike in caloric needs. Similarly, during periods of illness or post-vaccination recovery, babies may nurse longer or more often for both nutrition and comfort. These surges in demand are essential for stimulating the mother’s supply to match developmental needs. Allowing the newborn infant feeding process to remain responsive, rather than adhering to a rigid schedule, ensures that the baby’s changing physiological and emotional requirements are met without delay.
Navigating Weaning: How long should infants breastfeed in relation to introducing cow’s milk or plant-based alternatives?
As babies approach their first birthday, parents begin to consider weaning from breast milk to other forms of milk, such as cow’s milk or fortified plant-based alternatives. However, questions arise around how long should infants breastfeed before transitioning without sacrificing nutritional integrity. Most pediatricians recommend continuing breastfeeding for at least the first year and supplementing with solid foods that include iron, calcium, and healthy fats. If breastfeeding continues beyond one year, the need for cow’s milk may be reduced, as breast milk remains nutritionally dense and well-absorbed. When choosing plant-based options, it’s essential to ensure that the product is fortified with vitamin D, B12, and calcium, as unfortified versions may not meet a toddler’s dietary needs.
How long breast feed patterns influence postpartum maternal health and recovery
Breastfeeding triggers the release of oxytocin, which assists the uterus in returning to its pre-pregnancy size and helps minimize postpartum bleeding. The act of nursing also contributes to a delay in the return of ovulation and menstruation, which can naturally space pregnancies. Furthermore, women who breastfeed for longer durations tend to have lower lifetime risks of breast and ovarian cancers, type 2 diabetes, and cardiovascular disease. Exploring how long breast feed patterns impact maternal well-being reveals that the benefits are reciprocal: breastfeeding supports both the child’s and mother’s health in profound ways. These outcomes underscore the need for broader societal support to extend breastfeeding opportunities and reduce premature weaning due to lack of accommodations.
How long should you breastfeed if your baby is in childcare or shared custody situations?
For parents navigating shared custody or daily childcare, sustaining breastfeeding requires additional coordination but remains entirely feasible. Determining how long should you breastfeed under these conditions depends on maintaining milk supply through pumping and establishing consistent routines that allow for nursing during transition times. Breastfeeding can become a meaningful ritual at pick-up and drop-off, providing emotional grounding and helping ease separation anxiety. Labeling expressed milk carefully and storing it in adequate volumes helps caregivers maintain feeding continuity. Additionally, ongoing communication between all adults involved ensures that newborn infant feeding protocols are respected, and that the infant’s nutritional and comfort needs remain at the center of caregiving decisions.
Adapting to Baby-Led Weaning: When do infants stop eating every 3 hours once solids are introduced?
With the introduction of baby-led weaning—a method that allows infants to self-feed solid foods rather than relying on spoon-feeding—feeding intervals often shift organically. While traditional feeding schedules may space out over time, babies navigating this method may still nurse frequently to supplement their intake, especially as they experiment with food textures. Observing when do infants stop eating every 3 hours can help parents track readiness for longer stretches between meals and improved self-regulation. It’s important to remember that during the initial stages of baby-led weaning, most of the infant’s caloric intake still comes from breast milk. Nursing on demand remains essential for ensuring that nutritional gaps are filled while the baby learns to chew, swallow, and accept a variety of solid foods at their own pace.
Conclusion: Embracing Individual Journeys While Understanding How Long Should Infants Breastfeed
Determining how long should infants breastfeed is a deeply personal decision informed by medical guidance, cultural context, and family dynamics. There is no singular answer that fits every child, but there is a wealth of evidence pointing to the profound benefits of sustained breastfeeding for immune protection, neurological development, and emotional wellbeing. By recognizing the value of exclusive breastfeeding in the early months and embracing its ongoing contributions through the toddler years, caregivers can make empowered choices that support their child’s optimal growth.
Navigating questions such as how long should a newborn feed for, how long do babies breastfeed, and when do infants stop eating every 3 hours can be overwhelming, but understanding the science behind infant feeding patterns provides clarity. Parents deserve compassionate, evidence-based support as they balance the ideal with the realities of daily life. Whether breastfeeding for six months, one year, or beyond, what matters most is a nurturing, responsive approach that centers the baby’s needs and the family’s wellbeing. In doing so, families lay the foundation for lifelong health, resilience, and connection.
Further Reading:
Continued breastfeeding for healthy growth and development of children