Introduction
Gastrointestinal health is foundational to overall well-being, yet it is one of the most commonly misunderstood and overlooked aspects of health. Every day, millions of people silently endure discomforts like bloating, cramping, acid reflux, and irregular bowel habits, often brushing them off as temporary or insignificant. But beneath these routine complaints may lie more serious conditions. Understanding the full spectrum of GI symptoms and disorders—ranging from functional issues to chronic diseases—can make the difference between early intervention and prolonged suffering.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
The gastrointestinal system includes a series of connected organs responsible for processing food, absorbing nutrients, and expelling waste. It also plays a critical role in immune regulation, hormone production, and even mental health, thanks to the intricate communication pathway known as the gut-brain axis. When any part of this complex system is compromised, the effects ripple across multiple dimensions of health. From mild digestive upset to signs of systemic dysfunction, gastrointestinal issues demand attention and understanding.
In this article, we explore the many faces of gastrointestinal distress. We’ll break down what gastrointestinal disease looks like in real life, examine the earliest warning signs that something deeper may be wrong, and uncover what causes these disorders in the first place. You’ll learn how stomach and colon illnesses differ, how upper GI disorders present compared to lower GI problems, and how to identify the subtle symptoms that often precede more severe diagnoses. With expert-backed guidance and science-based clarity, this comprehensive guide will help you decode what your digestive system is trying to tell you—and how to support it more intelligently moving forward.
What Does GI Mean in Medical Terms?
In medical terminology, the abbreviation “GI” refers to the gastrointestinal tract, a continuous system of hollow organs extending from the mouth to the anus. These include the esophagus, stomach, small intestine, large intestine (also called the colon), and rectum. While the digestive process begins in the mouth, the real work of digestion and absorption happens as food passes through the GI tract, particularly in the stomach and intestines. Accessory organs like the liver, pancreas, and gallbladder also play key roles, producing enzymes, bile, and other substances necessary for efficient digestion.
Understanding what GI means is crucial when discussing gastrointestinal issues. GI symptoms encompass a vast array of digestive complaints, and GI disorders may involve any part of the system, including inflammatory, infectious, functional, and structural conditions. From heartburn and nausea to more severe problems like ulcerative colitis or colorectal cancer, the GI system is vulnerable to many forms of distress. Learning the language of gastrointestinal medicine can help patients become better advocates for their health, allowing them to articulate symptoms clearly and pursue timely intervention.
Early Signs of Gastrointestinal Disease
One of the greatest challenges in diagnosing gastrointestinal disease lies in its subtle onset. The early signs are often vague, nonspecific, and easy to dismiss. Many people begin with occasional bloating, mild discomfort after meals, or intermittent constipation and assume these symptoms are normal. But when these issues persist or begin to interfere with daily life, they can signify the early stages of more serious gastrointestinal conditions.
Symptoms such as frequent indigestion, gas, irregular bowel movements, nausea, and unexplained fatigue may point to inflammation, microbial imbalance, or nutrient malabsorption. These early signals are often the body’s first warnings that the digestive system is under strain. Left unchecked, these initial problems can evolve into full-blown gastrointestinal disorders with systemic effects, affecting skin, mood, energy levels, and immune resilience.
Recognizing the early signs of gastrointestinal disease requires heightened body awareness and a willingness to take persistent symptoms seriously. Early medical evaluation can help identify imbalances and structural issues before they progress. For individuals at risk—due to family history, stress, medication use, or dietary habits—being proactive about digestive health is one of the most effective forms of preventive care.
Common Gastrointestinal Symptoms and What They Indicate
Gastrointestinal symptoms are among the most commonly reported health concerns in clinical settings, yet their significance varies widely. Some are benign and fleeting, while others indicate chronic or progressive disease. Understanding how to interpret symptoms like abdominal pain, bloating, diarrhea, constipation, reflux, and nausea is essential for distinguishing between functional complaints and signs of underlying pathology.
Abdominal pain can reflect everything from mild gas to appendicitis or diverticulitis. Bloating may arise from overeating, food intolerances, or small intestinal bacterial overgrowth (SIBO). Diarrhea could be caused by a viral infection or an inflammatory bowel disease. Constipation might result from dehydration, low fiber intake, or a thyroid disorder. When GI symptoms are persistent, worsening, or accompanied by weight loss, fatigue, or rectal bleeding, a more thorough investigation is warranted.
The gut’s connection to the immune system and brain means that gastrointestinal issues can manifest systemically. Changes in mood, cognition, or skin health may also be related to digestive dysfunction. When the body absorbs nutrients inefficiently or when inflammation is chronic, symptoms extend beyond the GI tract. By mapping symptom patterns to possible causes, healthcare providers can develop more precise diagnostic and treatment plans.
What Digestive Disorders Occur in the Stomach?
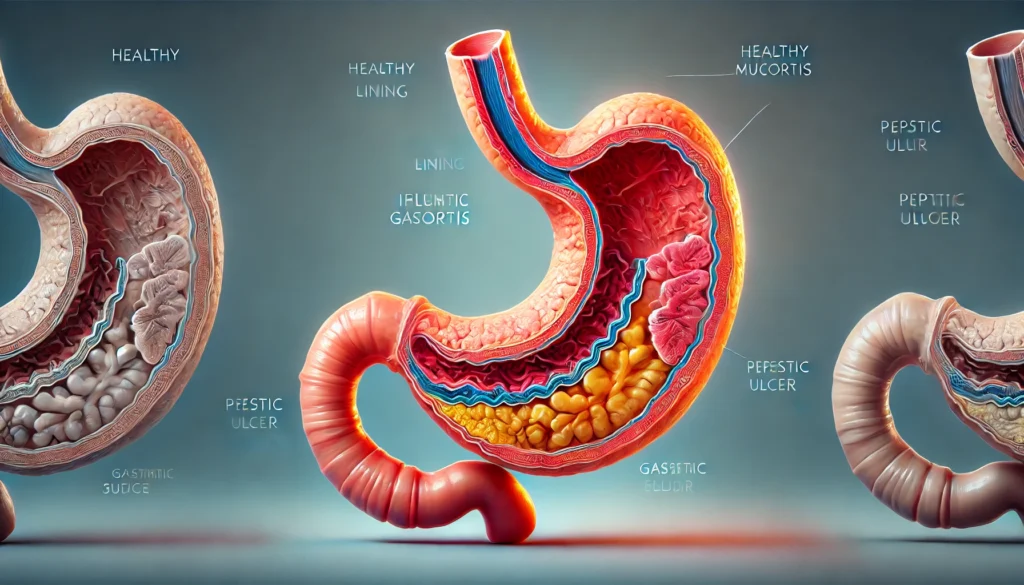
Several well-documented disorders occur specifically in the stomach, each with unique presentations and risks. Gastritis is one of the most common, involving inflammation of the stomach lining often caused by infection with Helicobacter pylori, prolonged NSAID use, or alcohol consumption. It can cause burning pain, nausea, and a sensation of fullness after small meals. If untreated, gastritis may lead to ulcers or even gastric cancer.
Peptic ulcer disease results from acid erosion of the stomach or duodenal lining. It often causes gnawing or burning pain, especially when the stomach is empty. Some ulcers bleed, leading to black, tarry stools or vomiting blood. GERD, or gastroesophageal reflux disease, occurs when acid from the stomach flows back into the esophagus, causing heartburn, regurgitation, and in some cases, damage to the esophageal lining.
Functional dyspepsia refers to upper GI discomfort without a clear structural cause. It can include sensations of pressure, pain, early satiety, or bloating, and is often linked to stress or eating habits. Though these stomach disorders vary in severity, all benefit from timely medical evaluation and nutritional management to reduce progression and improve quality of life.

Diseases of the Colon and Lower GI Tract
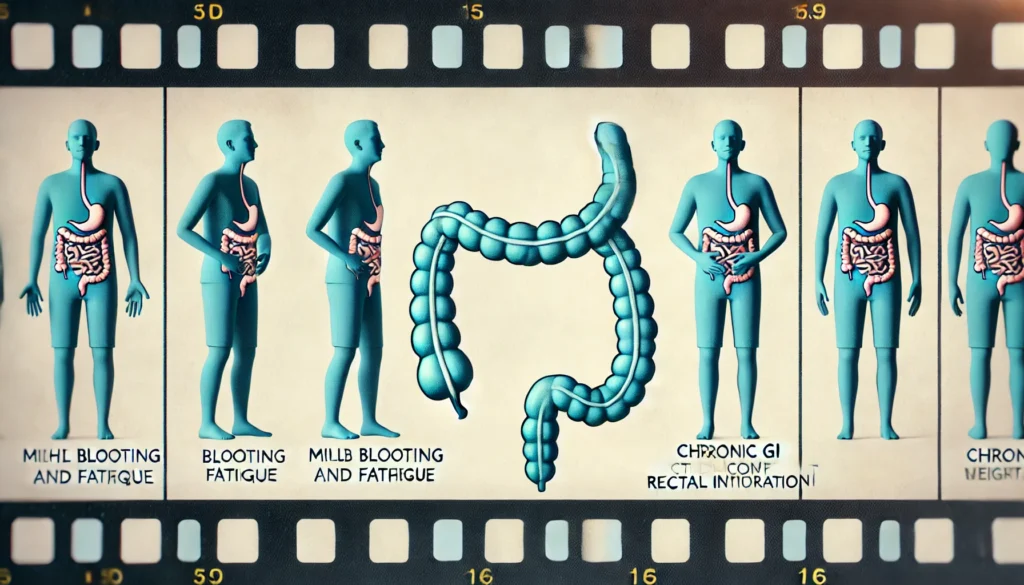
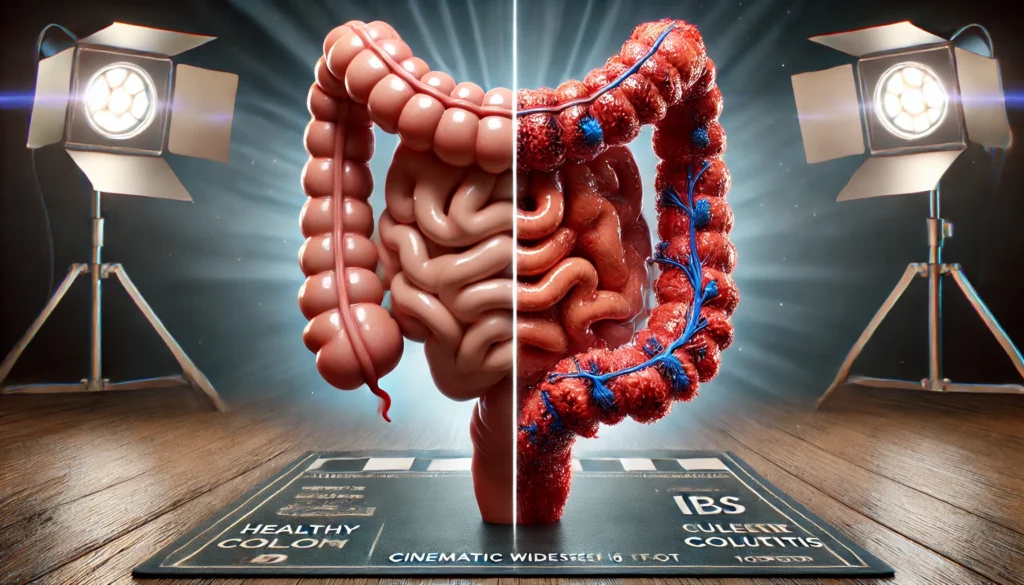
The colon and lower gastrointestinal tract are commonly affected by a range of conditions that can disrupt bowel habits, trigger inflammation, or in severe cases, lead to life-threatening complications. Among the most recognized are ulcerative colitis and Crohn’s disease, both forms of inflammatory bowel disease (IBD). These autoimmune disorders cause chronic inflammation and ulceration in the colon, leading to pain, bleeding, fatigue, and diarrhea.
Irritable bowel syndrome (IBS) is a functional disorder characterized by abdominal discomfort, bloating, and fluctuating bowel patterns, but without visible inflammation or damage. Though considered less serious than IBD, IBS can severely impact quality of life and may require long-term dietary and behavioral strategies for symptom control.
Diverticulosis, the development of small pouches in the colon wall, is common in older adults and may progress to diverticulitis when these pouches become inflamed or infected. Symptoms include lower abdominal pain, fever, and changes in bowel habits. Colorectal cancer is another critical concern, often developing silently over time before manifesting with blood in the stool, anemia, or unexplained weight loss.
Understanding diseases of the colon is vital, particularly as these conditions often progress silently until advanced. Regular screening, especially after the age of 45, and early attention to bowel changes can significantly reduce risks and support long-term colon health.
What Are the 5 Major Digestive System Diseases?
While many digestive diseases exist, five conditions are particularly common and well-documented in clinical literature. Gastroesophageal reflux disease (GERD) affects millions worldwide, causing chronic acid reflux and increasing the risk of esophageal damage. Peptic ulcer disease, caused by acid erosion or infection, creates painful sores in the stomach or upper intestine and may lead to internal bleeding.
Celiac disease is an autoimmune disorder triggered by gluten, leading to damage in the small intestine and nutrient malabsorption. Inflammatory bowel disease, encompassing both Crohn’s disease and ulcerative colitis, leads to chronic inflammation, weight loss, and debilitating symptoms. Irritable bowel syndrome, though non-inflammatory, causes significant abdominal discomfort and altered bowel function, often linked to stress and food sensitivities.
Together, these five diseases represent a wide range of digestive pathology—from structural to functional, inflammatory to immune-mediated. Each requires a tailored treatment plan that includes dietary adjustments, medications, stress management, and sometimes surgical intervention.
Causes of Digestive Problems and Systemic Triggers
Digestive disorders can arise from many causes, often involving an interplay of genetics, environment, lifestyle, and microbial imbalance. Poor diet is among the most influential factors, particularly one high in processed foods, artificial additives, trans fats, and refined sugars. These dietary habits can compromise the intestinal barrier, disrupt gut flora, and promote systemic inflammation.
Infections, including viruses, parasites, and pathogenic bacteria, can alter gut function and trigger chronic post-infectious syndromes. Overuse of medications like antibiotics, NSAIDs, and proton-pump inhibitors may also weaken the gut lining or destroy beneficial microbes. Stress is another major player—chronic stress alters gut motility, increases permeability, and suppresses immune function in the gastrointestinal tract.
Food intolerances, including those related to lactose, fructose, or gluten, can provoke inflammation and symptom flare-ups in susceptible individuals. Autoimmune diseases, genetic predispositions, and hormonal imbalances also contribute to digestive issues, creating a perfect storm for chronic GI distress. Identifying and addressing root causes—rather than masking symptoms—paves the way for meaningful healing and lasting resolution.
Frequently Asked Questions
1. What is gastrointestinal disease and how is it diagnosed?
Gastrointestinal disease encompasses any condition affecting the digestive tract, from the esophagus to the colon. It includes structural, functional, inflammatory, and neoplastic disorders. Diagnosis typically begins with a detailed symptom history and physical exam, followed by blood tests, stool analysis, imaging scans, endoscopy, and sometimes biopsy. The goal is to identify inflammation, infections, bleeding, structural abnormalities, or signs of autoimmune activity. A tailored approach to diagnosis ensures that both common and rare conditions are evaluated and addressed with appropriate treatment.
2. What are the most common symptoms of gastrointestinal disorders?
The most frequently reported GI symptoms include abdominal pain, bloating, gas, heartburn, constipation, diarrhea, nausea, vomiting, and irregular bowel movements. Some individuals may also experience fatigue, weight loss, skin issues, or mood changes due to nutrient deficiencies or gut-brain axis disruption. When these symptoms are persistent, worsen over time, or impact quality of life, they may signal an underlying gastrointestinal disorder that requires medical attention.
3. What are upper GI disorders and how do they differ from lower GI issues?
Upper GI disorders affect the esophagus, stomach, and duodenum. Common examples include GERD, gastritis, ulcers, and functional dyspepsia. These conditions often present with heartburn, chest discomfort, early satiety, or nausea. Lower GI disorders involve the small intestine, colon, and rectum, with symptoms such as abdominal cramping, diarrhea, constipation, and rectal bleeding. Understanding the anatomical location of symptoms helps guide diagnostic strategies and treatment protocols, ensuring more precise care.
4. What causes gastrointestinal symptoms to persist chronically?
Chronic GI symptoms can result from unaddressed infections, long-term inflammation, autoimmune activation, or dysbiosis—an imbalance in gut microbes. Psychological stress and unresolved trauma can also contribute by disrupting gut-brain communication. Medications, poor diet, and food intolerances are additional culprits. When symptoms persist for weeks or months, it’s essential to explore all potential root causes rather than relying solely on temporary relief through symptom-suppressing medications.
5. What does the stomach issue look like in adults?
Stomach issues in adults often appear as persistent upper abdominal discomfort, burning pain after meals, bloating, or a sensation of fullness even with small portions. Nausea, burping, sour taste in the mouth, or food coming back up into the throat may suggest acid reflux or ulcers. More severe cases may involve vomiting blood, black stools, or unintended weight loss—signs that indicate a need for urgent medical evaluation. Understanding these patterns helps distinguish minor complaints from potentially serious gastric diseases and symptoms.
6. Are colon illnesses different from other gastrointestinal conditions?
Colon illnesses are specific to the large intestine and include conditions such as ulcerative colitis, diverticulitis, colorectal cancer, and IBS. They differ in both symptoms and pathology from diseases affecting the stomach or small intestine. Colon-related issues often present with lower abdominal pain, rectal bleeding, constipation, or urgent diarrhea. Early detection through screening colonoscopy and prompt response to changes in bowel habits are vital for effective treatment and prevention of complications.
7. What are signs of gastrointestinal disorders that need urgent care?
Warning signs include unintentional weight loss, persistent vomiting, black or bloody stools, severe or unrelenting abdominal pain, and prolonged changes in bowel habits. These symptoms may suggest bleeding ulcers, malignancies, or inflammatory diseases that require immediate intervention. Other red flags include iron-deficiency anemia, jaundice, or fever accompanying digestive symptoms. Any combination of these warrants thorough investigation to rule out life-threatening causes.
8. Which digestive disorders affect the stomach most commonly?
The most common stomach-related disorders include gastritis, gastric ulcers, GERD, and in some cases, gastric cancer. These conditions result from factors like acid overproduction, bacterial infection, chronic NSAID use, or autoimmune gastritis. Typical symptoms involve gnawing pain, heartburn, nausea, vomiting, and early satiety. Diagnosis often involves endoscopy and biopsy to assess mucosal integrity and rule out malignancy.
9. How is a digestive disorder different from occasional indigestion?
Occasional indigestion is often transient and linked to food choices, stress, or overeating. It typically resolves on its own. A digestive disorder, on the other hand, involves recurring or chronic symptoms that may reflect structural damage, inflammation, or systemic imbalance. These conditions often require clinical testing, medical intervention, and long-term management strategies to achieve resolution and prevent complications.
10. Is “poor man’s GI disease” a real condition?
The term “poor man’s GI disease” is often used informally to describe conditions like IBS or functional dyspepsia, where patients experience significant distress but lack objective findings on conventional tests. While the term is not medically recognized, the conditions it refers to are real and can severely impact daily life. These disorders often respond best to holistic, personalized approaches that include dietary changes, stress management, and gut-brain axis support.

Conclusion
Gastrointestinal health lies at the heart of human vitality, touching everything from immunity and cognition to mood and metabolism. Understanding the symptoms, triggers, and diseases that affect the GI tract can transform how we approach both prevention and treatment. Whether you’re managing bloating and discomfort or exploring the deeper causes of chronic illness, knowledge is your greatest ally.
By recognizing early signs, seeking timely diagnosis, and addressing root causes—not just symptoms—you empower yourself to build a foundation of resilience. GI disorders may start subtly, but their consequences can be far-reaching. When we listen to the body’s messages, support the gut with smart choices, and seek medical guidance when needed, healing becomes not only possible but inevitable.
The path to digestive wellness begins with awareness. And from awareness, we find the strength to restore, rebalance, and reclaim our health from the inside out.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.