Introduction
Gastrointestinal infection is a common yet potentially severe condition that affects millions worldwide each year. Often underestimated due to its sometimes mild and self-limiting symptoms, this category of illness encompasses a wide range of infectious gut diseases that can significantly disrupt digestive function, nutrient absorption, and overall health. From sudden bouts of diarrhea while traveling to more chronic infections that linger undetected for weeks, understanding the full scope of gastrointestinal infections is essential for effective diagnosis, prevention, and care.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
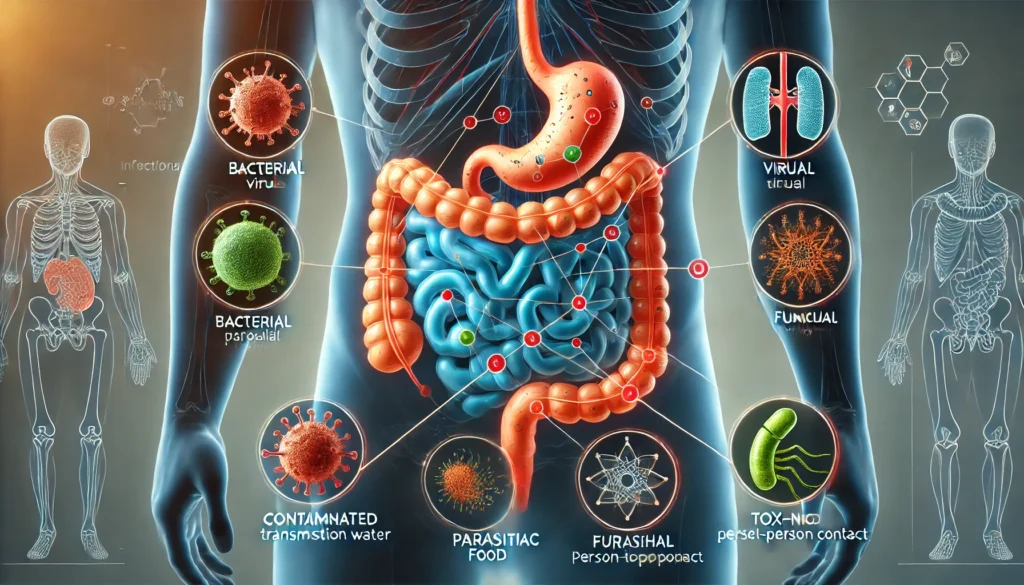
These infections can be caused by a diverse group of pathogens, including bacteria, viruses, parasites, and fungi. Each pathogen type has its own profile of symptoms, modes of transmission, and treatment strategies. The body’s gastrointestinal tract, especially the stomach and intestines, is particularly vulnerable to contamination through food, water, or poor hygiene practices. As such, outbreaks can affect not only individuals but entire communities, leading to significant public health concerns.
Infectious gut diseases are not only limited to severe epidemics or tropical pathogens. Many intestinal infection names are recognizable to patients across every demographic—from norovirus and rotavirus to giardiasis and salmonella. These illnesses can strike unexpectedly, often leading to acute symptoms such as vomiting, abdominal cramps, and watery diarrhea. However, in vulnerable populations like children, older adults, and those with compromised immune systems, even mild infections can result in hospitalization or long-term health complications.
This article explores the detailed biology, causes, symptoms, and treatments for gastrointestinal infections. We will examine how these infections spread, the common and rare intestinal infection names clinicians encounter, and what makes some people more susceptible than others. Our goal is to provide a comprehensive understanding rooted in science, supported by medical research, and applicable to real-life prevention and care. Whether you’re dealing with symptoms now, recovering from a recent illness, or aiming to protect your gut health long-term, this guide delivers trusted insights into every aspect of infectious gut diseases.

Understanding Gastrointestinal Infections: A Scientific Overview
Gastrointestinal infections refer to inflammatory conditions caused by infectious agents in the gastrointestinal tract. These include the stomach, small intestine, and large intestine. The infection typically begins after ingestion of contaminated food, water, or by contact with infected individuals. Once inside the gut, pathogens disrupt the natural balance of gut flora, damage mucosal linings, and elicit immune responses that lead to the hallmark symptoms of diarrhea, nausea, and cramping.
Bacteria are among the most well-known causes of gastrointestinal infection. Species such as Escherichia coli (E. coli), Salmonella, Campylobacter, and Shigella can lead to serious foodborne illnesses. Viruses, particularly norovirus and rotavirus, are common in both pediatric and adult populations and are highly contagious. Parasites, including Giardia lamblia and Entamoeba histolytica, are often acquired through contaminated water and are more prevalent in developing regions, though they are not uncommon in industrialized nations.
Each of these pathogens has evolved specific mechanisms for surviving gastric acid, attaching to intestinal cells, and evading immune defenses. In some cases, they release toxins that further damage tissues and disrupt fluid regulation in the intestines, leading to dehydration and electrolyte imbalance. The body responds with inflammation, increased gut motility, and heightened immune activity—all of which contribute to symptom severity.
Diagnosis requires careful clinical history, symptom assessment, and often laboratory testing such as stool cultures, antigen tests, or PCR panels. While many infections are self-limiting, others require targeted antibiotic, antiviral, or antiparasitic treatment. In some instances, hospitalization becomes necessary due to complications like bloody diarrhea, sepsis, or severe dehydration.
Understanding these biological mechanisms is crucial not only for treatment but also for prevention. With the rise of antimicrobial resistance, climate change, and global travel, the landscape of infectious gut diseases is evolving. By delving into the science of gastrointestinal infection, we gain the tools to anticipate, manage, and mitigate its wide-ranging effects on human health.

Intestinal Infection Names: The Most Common and Dangerous Pathogens
The names of intestinal infections reflect both the pathogen involved and the symptoms they trigger. Some have become household names due to frequent news coverage or personal experience, while others remain lesser-known despite their impact. Let’s explore some of the most frequently encountered intestinal infection names and their clinical significance.
Norovirus is arguably the most common cause of viral gastroenteritis worldwide. Known for causing outbreaks in schools, cruise ships, and healthcare facilities, norovirus spreads rapidly through close contact or contaminated surfaces. Symptoms include sudden vomiting, watery diarrhea, fever, and malaise. While usually self-limiting, it poses a higher risk for elderly and immunocompromised patients.
Rotavirus primarily affects infants and young children, often resulting in hospitalization due to dehydration. Though vaccines have dramatically reduced its prevalence, rotavirus remains a significant cause of gastrointestinal infection in countries without widespread immunization.
Salmonella and Campylobacter are leading bacterial causes of foodborne illness. These bacteria are commonly transmitted through undercooked poultry, eggs, and contaminated produce. Symptoms of these infectious gut diseases include abdominal cramping, diarrhea (often bloody), and fever. Some strains can cause invasive disease, spreading beyond the intestine to joints or the bloodstream.
E. coli, particularly the O157:H7 strain, is infamous for producing Shiga toxins that can cause hemolytic uremic syndrome (HUS), a life-threatening condition involving kidney failure. It is typically associated with undercooked beef and unpasteurized juices.
Giardia lamblia is a protozoan parasite responsible for giardiasis. Often contracted from lakes, streams, or poorly treated drinking water, it causes prolonged diarrhea, bloating, and malabsorption. Giardia infection can become chronic and is known to impact growth and development in children.
Entamoeba histolytica is another serious parasitic agent, capable of causing amebiasis with potential for liver abscesses. It is more prevalent in tropical areas but may occur in travelers or immigrants.
Clostridioides difficile (C. difficile) is a unique gastrointestinal infection often resulting from antibiotic use. It disrupts the natural microbiome, leading to toxin-mediated colitis, severe diarrhea, and potential fatal complications if untreated.
These intestinal infection names represent a broad spectrum of pathogens, each with distinct challenges. From diagnosis to treatment, understanding the causative organism is essential for appropriate management and prevention of recurrence.

Transmission and Risk Factors: How Gastrointestinal Infections Spread
Understanding how gastrointestinal infections spread is fundamental for controlling outbreaks and preventing personal illness. Most infectious gut diseases follow fecal-oral transmission, which occurs when microscopic fecal particles from an infected individual are ingested—typically through contaminated food, water, or unwashed hands.
Poor sanitation and hygiene are the primary enablers of transmission. In low-resource settings, open defecation and lack of clean water dramatically increase exposure. In more developed environments, transmission often occurs in group settings such as daycare centers, nursing homes, restaurants, and hospitals.
Food safety plays a critical role. Undercooked meat, raw shellfish, unwashed produce, and unpasteurized dairy are common vehicles for bacterial gastrointestinal infection. Cross-contamination in kitchens—using the same cutting board for raw chicken and vegetables, for instance—can rapidly spread pathogens.
Waterborne transmission is also a major concern. Natural bodies of water can harbor parasites like Giardia, especially in regions lacking water treatment infrastructure. Even municipal water systems can fail, as seen in some recent E. coli outbreaks. Boiling or filtering water when traveling is often necessary to prevent intestinal infection.
Certain individuals face higher risks. These include infants, elderly adults, people with compromised immunity, and those on antibiotics or immunosuppressive medications. Travelers to developing countries also face increased exposure to infectious gut diseases, often referred to as traveler’s diarrhea. Immunity plays a role too; people repeatedly exposed to certain pathogens (e.g., children in daycare) may develop partial immunity over time.
Personal hygiene—especially handwashing with soap and water—is one of the most effective preventive measures. Safe food handling, proper cooking temperatures, clean drinking water, and sanitation infrastructure also significantly reduce risk. Education on how gastrointestinal infections spread empowers individuals and communities to interrupt transmission pathways and build healthier environments.
Symptoms of Infectious Gut Diseases: From Mild to Life-Threatening
The clinical presentation of gastrointestinal infection can range from mild and self-limiting to rapidly progressive and dangerous. While each pathogen may present a slightly different symptom profile, common symptoms often include nausea, vomiting, abdominal cramping, bloating, fever, and diarrhea. The duration, severity, and accompanying signs help clinicians differentiate among types of infections and guide appropriate treatment.
Acute watery diarrhea is the hallmark symptom of most viral gastrointestinal infections, including norovirus and rotavirus. Vomiting often accompanies diarrhea in viral cases, with symptoms typically resolving within 1 to 3 days. Fever and generalized malaise are common, particularly in children.
Bacterial infections often cause more intense symptoms. In addition to diarrhea—which may be bloody—patients may experience high fever, persistent abdominal pain, and dehydration. Shigella and Campylobacter can mimic inflammatory bowel disease, while Salmonella may lead to systemic infection requiring antibiotics.
Parasitic infections tend to produce more chronic gastrointestinal symptoms. Giardia lamblia causes greasy, foul-smelling stools, bloating, and weight loss. Entamoeba histolytica can lead to severe dysentery, liver abscesses, and long-term fatigue. The gradual onset and prolonged duration of symptoms often lead to delayed diagnosis.
Dehydration is a serious concern with any gastrointestinal infection. Symptoms include dry mouth, decreased urination, sunken eyes, and rapid heartbeat. Children and older adults are particularly vulnerable to fluid loss. In extreme cases, dehydration can lead to kidney failure, seizures, or death.
A subset of patients may experience post-infectious complications. These include reactive arthritis, irritable bowel syndrome, or prolonged nutrient malabsorption. Recognizing the diverse symptom spectrum of infectious gut diseases ensures early treatment and limits potential complications.
Diagnosis of Gastrointestinal Infection: Tests and Tools
Diagnosing gastrointestinal infection begins with a detailed clinical history and symptom timeline. Questions about recent travel, food exposure, sick contacts, and hygiene practices help narrow down potential pathogens. Physical examination often reveals abdominal tenderness, signs of dehydration, or in severe cases, systemic toxicity.
Laboratory testing is essential for definitive diagnosis, particularly when symptoms are severe, persistent, or atypical. Stool samples are the most common diagnostic tool. These samples may be tested for white blood cells, culture for bacterial pathogens, or evaluated using antigen detection and polymerase chain reaction (PCR) assays to identify viral and parasitic agents.
Rapid antigen tests are useful for detecting rotavirus, norovirus, and some parasitic infections. PCR panels can simultaneously detect multiple pathogens, offering a comprehensive look at infectious causes within hours. These tools have improved both speed and accuracy of gastrointestinal infection diagnosis.
In cases where invasive disease is suspected, blood tests may show elevated white cell counts, markers of inflammation, or anemia. Liver function tests and imaging such as ultrasound or CT scan may be required if complications like liver abscess or perforation are suspected.
Endoscopy is not typically needed for routine infectious gut diseases but may be used when structural damage, chronic symptoms, or differential diagnosis with inflammatory bowel disease is necessary.
Accurate diagnosis not only directs the appropriate treatment but also informs public health decisions, especially during outbreaks. Identifying the specific pathogen helps track sources, contain transmission, and educate patients on prevention strategies.
Frequently Asked Questions
1. What is a gastrointestinal infection and how does it differ from other digestive issues?
A gastrointestinal infection is caused by pathogens such as bacteria, viruses, or parasites that invade and disrupt the digestive tract. Unlike chronic digestive issues like IBS or IBD, which are often non-infectious and linked to immune or functional disorders, gastrointestinal infections are acute and triggered by exposure to harmful microorganisms. These infections often have sudden onset, and symptoms like diarrhea, vomiting, and fever distinguish them from non-infectious digestive conditions. Proper identification is crucial for treatment, as some infections resolve on their own while others require medical intervention.
2. What are the most common intestinal infection names patients should know?
Familiar intestinal infection names include norovirus, rotavirus, Salmonella, E. coli, Shigella, Campylobacter, Giardia, and Entamoeba histolytica. These infections differ in severity and transmission, but all affect the gastrointestinal tract. Knowing these names helps patients understand the nature of their illness, ask informed questions, and follow appropriate preventive steps. Awareness also aids in recognizing symptoms early and seeking timely care to avoid complications such as dehydration or chronic gastrointestinal distress.
3. How do infectious gut diseases typically spread from one person to another?
Most infectious gut diseases spread through the fecal-oral route. This means that microscopic amounts of fecal matter from an infected person are ingested by another—often through contaminated food, water, surfaces, or hands. Poor sanitation, inadequate hand hygiene, and improper food handling are the most common transmission methods. Viral infections like norovirus can also spread via aerosolized vomit particles, increasing the risk in crowded spaces. Understanding transmission routes helps break the infection cycle and informs best practices in hygiene and food safety.
4. Who is most at risk for gastrointestinal infection complications?
Infants, elderly individuals, immunocompromised patients (including those with HIV or undergoing chemotherapy), and people with chronic illnesses are at higher risk for complications. In these populations, gastrointestinal infections can cause more severe dehydration, nutrient deficiencies, or secondary infections. Pregnant women may also face higher risks depending on the pathogen. Travelers to regions with limited access to clean water or sanitation are additionally vulnerable. Extra vigilance in hygiene, food selection, and preventive vaccination (where available) is crucial for these groups.
5. What symptoms suggest a gastrointestinal infection is severe?
Severe gastrointestinal infection symptoms include high fever, persistent vomiting, signs of dehydration (dry mouth, low urine output, sunken eyes), blood or mucus in stool, and rapid weight loss. When these symptoms occur, medical evaluation is necessary. Prolonged diarrhea lasting more than three days, severe abdominal pain, and altered mental status are also red flags. In infants or older adults, any gastrointestinal symptoms can quickly become serious, making early intervention critical to prevent hospitalization or long-term complications.
6. Can gastrointestinal infections cause long-term health problems?
Yes, some gastrointestinal infections can lead to long-term consequences. Post-infectious irritable bowel syndrome (PI-IBS) is a known complication, especially following bacterial infections. Reactive arthritis, Guillain-Barré syndrome (after Campylobacter), and chronic fatigue are also documented in some patients. Parasites like Giardia can cause prolonged malabsorption, affecting growth and development in children. Chronic inflammation from infections like Entamoeba may result in persistent gastrointestinal distress or liver complications. Prompt diagnosis and complete treatment reduce the likelihood of these outcomes.
7. How are infectious gut diseases treated and when are antibiotics used?
Treatment depends on the pathogen. Most viral infections resolve on their own with supportive care—hydration, rest, and electrolyte replacement. Bacterial infections may require antibiotics if symptoms are severe, prolonged, or involve high-risk patients. However, overuse of antibiotics can worsen certain infections, such as E. coli O157:H7, by increasing toxin release. Antiparasitic medications are prescribed for Giardia, Entamoeba, and other parasitic infections. Proper diagnosis ensures that treatment is targeted, effective, and avoids unnecessary medications.
8. Are there vaccines for gastrointestinal infections?
Yes, vaccines are available for some gastrointestinal infections. Rotavirus vaccines are routinely given to infants in many countries and have significantly reduced severe diarrheal illness. The oral cholera vaccine is available for travelers or during outbreaks. Ongoing research is developing norovirus vaccines, though none are yet approved for public use. Hepatitis A, a viral infection transmitted via contaminated food and water, also has an effective vaccine. Staying up to date on vaccines is an essential part of gut infection prevention.
9. How can I prevent gastrointestinal infection while traveling?
To prevent gastrointestinal infections during travel, especially to developing countries, drink only bottled or purified water, avoid raw fruits or vegetables unless you peel them yourself, and eat fully cooked food served hot. Avoid street food unless you observe strict hygiene. Wash hands frequently, especially before eating. Taking probiotics before and during travel may support gut resilience, though results vary. Consider vaccines like typhoid or hepatitis A when visiting high-risk areas. Travel clinics offer personalized preventive guidance.
10. What is the role of probiotics in preventing or treating gastrointestinal infections?
Probiotics may help prevent certain gastrointestinal infections by enhancing the natural gut microbiome, strengthening mucosal barriers, and outcompeting pathogens. Strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii are commonly used during or after antibiotic treatment to reduce the risk of C. difficile infection. They may also shorten the duration of viral diarrhea. However, not all probiotics are equal, and results depend on the strain, dose, and individual microbiome. Consult a healthcare provider before using probiotics therapeutically.

Conclusion
Gastrointestinal infection is more than just a passing stomach bug. It represents a dynamic interplay between pathogens, immune responses, and environmental exposures that can either resolve quickly or lead to lasting damage. Infectious gut diseases affect people of all ages and socioeconomic backgrounds, yet their symptoms are often dismissed or misdiagnosed. Recognizing the specific intestinal infection names, understanding how they spread, and knowing when to seek care are essential skills in today’s global health landscape.
From preventing common foodborne illnesses to navigating chronic parasitic infections, the science of gastrointestinal infection provides clear guidance for both individuals and communities. By adopting simple practices like handwashing, safe food preparation, clean water access, and timely vaccination, we can dramatically reduce the burden of these infections.
Empowering patients through education, encouraging clinicians to use precision diagnostics, and supporting public health efforts to improve sanitation are all part of the larger effort to protect digestive health. Whether you are recovering from an infection, caring for a loved one, or simply aiming to avoid illness, the key lies in informed action. Because when it comes to gut infections, what we know truly has the power to save lives—and restore health from the inside out.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Everything you need to know about gastrointestinal infections



