New parents often find themselves navigating a whirlwind of new experiences and information, especially when it comes to their infant’s health. Among the many concerns that may arise in those early months, questions about newborn skin conditions are both common and deeply personal. One of the most frequent inquiries posed by anxious parents is this: do newborns get allergies? This question reflects not only the growing awareness of allergy-related health concerns in children but also the understandable confusion about what is normal versus what may signal an underlying issue. While the concept of allergies might seem premature in the context of a brand-new life, emerging research and clinical insights tell us that even the youngest babies can exhibit signs of allergic sensitivity. From puzzling rashes to digestive disturbances, the signs can vary widely—yet understanding them is essential for supporting a child’s long-term health, especially in the context of nutrition and food exposure.
You may also like: The Ultimate Guide to Choosing the Best Sippy Cup for Healthy Hydration and Growing Kids
Understanding Infant Skin and Immune Development
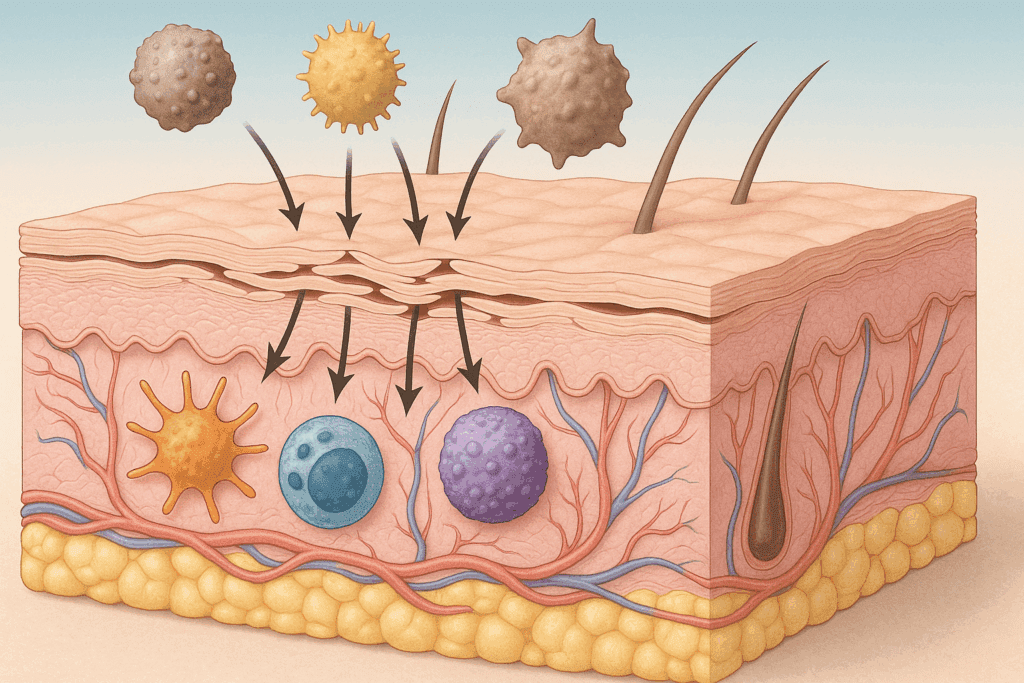
To appreciate why allergies might show up in the earliest stages of life, it’s crucial to understand the nature of a newborn’s skin and immune system. At birth, an infant’s skin barrier is thinner, more permeable, and less resilient than an adult’s, making it particularly sensitive to environmental irritants. The outermost layer of the skin, known as the stratum corneum, continues to mature during the first year of life. This developmental process is vital because an immature skin barrier can allow allergens and microbes to penetrate more easily, potentially triggering immune responses.
Simultaneously, the immune system of a newborn is still developing. Unlike adults, newborns rely heavily on maternal antibodies passed through the placenta and, after birth, through breast milk. These antibodies provide some initial protection, but they don’t necessarily prevent an allergic response. In fact, the neonatal immune system is unique in its design; it’s geared toward learning what to tolerate and what to defend against. This dual function—developing tolerance to harmless substances while preparing to battle pathogens—creates a delicate balance. When this balance tips unfavorably, it may explain why some babies develop food allergies, skin sensitivities, or other allergic symptoms during infancy.
Do Newborns Get Allergies? What Science Says About Early Sensitivities
The question “do newborns get allergies?” is more than a casual curiosity—it opens the door to understanding how early allergic responses are rooted in both genetics and environmental exposure. Clinically, allergies are defined as hypersensitive immune responses to substances that are typically harmless to most people. In newborns, these responses may be triggered by proteins in breast milk, formula ingredients, airborne particles, or even topical substances like skincare products. Studies have shown that even within the first few weeks of life, infants can display signs of allergic reactions such as eczema, digestive upset, or unusual fussiness following feeding.
Part of what makes this topic complex is that many of the signs of baby allergies mimic normal newborn behavior. For example, spitting up after feeds, crying, or rashes are common in all infants. However, when these symptoms are persistent, severe, or accompanied by other indicators such as wheezing, blood in the stool, or poor weight gain, it may suggest an underlying allergy. In such cases, infants and food allergies become a pressing concern requiring a tailored medical approach. The distinction between typical newborn behavior and pathological responses hinges on frequency, intensity, and the presence of patterns—elements that pediatricians are trained to assess thoroughly.

Signs of Allergies in Infants: How to Tell If Your Infant Has Allergies
Recognizing the early signs of allergies in infants requires careful observation and an understanding of how symptoms may manifest differently depending on the allergen involved. One of the most frequently discussed signs is a skin rash, which can appear as red, dry, itchy patches, often described clinically as atopic dermatitis or eczema. An infant food allergy rash typically appears on the cheeks, arms, or legs, and in some cases, may weep or crust over. Another important signal is gastrointestinal discomfort—babies with food allergies may exhibit vomiting, diarrhea, or constipation, and in severe cases, may present with blood-streaked stools.
Respiratory symptoms, though less common in newborns, can also be indicative of allergies. A stuffy nose, chronic sneezing, or wheezing may suggest that a baby is reacting to environmental allergens like dust mites or pet dander. It’s worth noting that these symptoms can also be attributed to infections, so persistent or unexplained respiratory issues should prompt a medical evaluation. In some situations, the infant may seem unusually irritable or have disrupted sleep, which are less specific symptoms but could be associated with discomfort from an allergic reaction. Parents wondering how to tell if baby is allergic to food should monitor for symptom patterns that appear after specific meals or feeding changes. This information is particularly useful for pediatricians attempting to narrow down possible triggers.

Exploring the Link Between Food Allergies in Babies and Skin Conditions
Food allergies in babies are not limited to digestive symptoms; in fact, skin manifestations are among the earliest and most telling signs. One of the most visible indicators is the infant food allergy rash, which may flare up shortly after consuming a specific formula or a breastfeeding mother’s ingestion of certain allergens. This reaction is generally a sign that the immune system is treating a food protein as a harmful substance, releasing histamines and other chemicals that provoke inflammation. As a result, skin reactions often co-occur with systemic symptoms such as fussiness, vomiting, or mucus in the stool.
The connection between food allergies and skin conditions also involves a concept known as the “atopic march”—a clinical progression in which infants with eczema or food allergies in early life may later develop allergic rhinitis or asthma. This sequence underscores the importance of early recognition and management of baby allergies, not only to address immediate discomfort but also to potentially mitigate long-term allergic risk. When examining a baby food allergy rash, pediatricians will consider factors such as its location, timing, and recurrence in relation to feeding. Differentiating these rashes from common skin issues like heat rash or baby acne requires clinical experience and, in some cases, diagnostic testing.

Can Infants Get Allergies from Breast Milk or Formula?
One of the more surprising revelations for many parents is that even breastfed babies can develop allergic responses, often through proteins passed into breast milk from the maternal diet. This raises the valid concern: can infants get allergies from what their mother eats? The answer is yes, although it’s relatively rare. When a breastfeeding mother consumes common allergens like dairy, soy, or peanuts, protein fragments from these foods can enter her milk and potentially trigger an allergic response in her infant. Signs that a baby may be reacting to something in breast milk include chronic gassiness, diarrhea, reflux, and skin rashes.
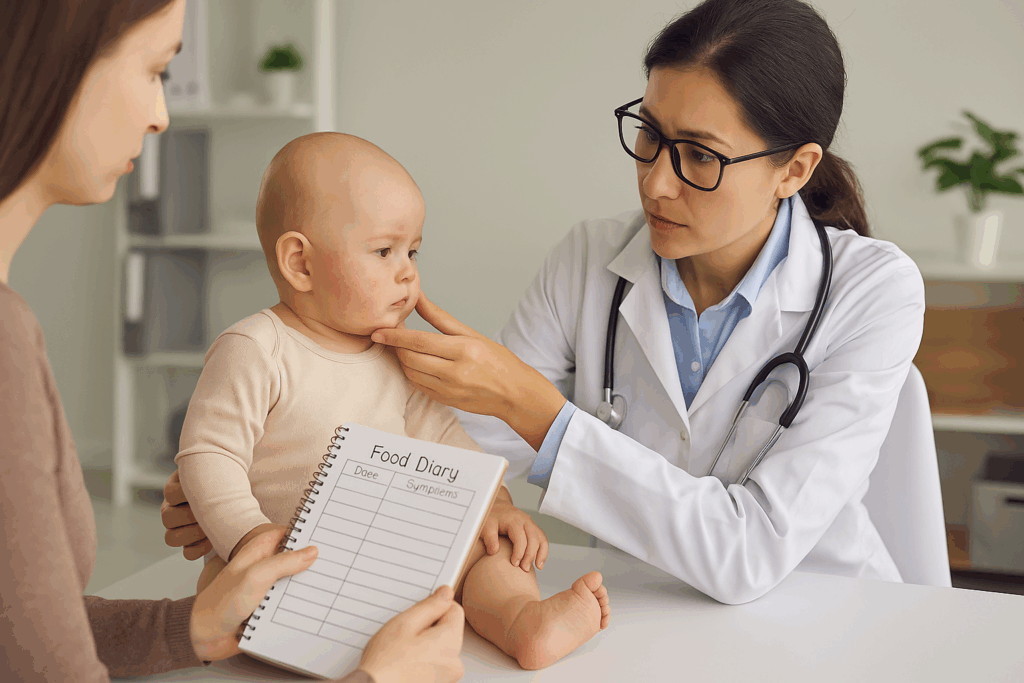
In formula-fed infants, the risk may be slightly higher, especially if the formula is based on cow’s milk or soy. In these cases, newborn food allergy symptoms might appear soon after starting a new formula and can include vomiting, poor feeding, and the appearance of an infant skin rash food allergy. For babies who show signs of intolerance or allergy, pediatricians may recommend switching to a hypoallergenic or extensively hydrolyzed formula. These formulas break down proteins into smaller fragments that are less likely to trigger an immune response. Understanding whether your baby is reacting to breast milk or formula can be a complex process, often requiring a careful food diary, symptom tracking, and expert guidance.
When Do Babies Develop Food Allergies and What Does It Mean for Feeding Practices?
The timeline for developing food allergies in babies is nuanced, with most allergic responses appearing within the first year of life. While some allergic tendencies may be present from birth, particularly if there is a family history of atopy (asthma, eczema, or hay fever), symptoms often become noticeable when solids are introduced. This critical transition, typically occurring around four to six months of age, is a time when parents are understandably vigilant about how to introduce allergens to baby. Current guidelines recommend introducing allergenic foods like eggs, peanuts, and fish early and gradually to promote tolerance rather than avoidance.
However, timing is only part of the equation. The way in which new foods are introduced—starting with small amounts, watching for reactions, and spacing out new additions—can significantly impact outcomes. Parents often ask how to know if baby is allergic to food during this phase. The answer lies in being observant, patient, and informed. Symptoms of an allergic reaction to new foods may include hives, vomiting, swelling of the lips or face, or a sudden change in behavior. A delayed reaction, such as an infant food allergy rash or increased irritability, may appear hours after consumption, complicating the diagnostic process.
Do Newborns Get Allergies Through Genetic or Environmental Exposure?
The interplay between genetics and environment is central to the question of how newborns get allergies. Studies suggest that if one parent has allergies, the child has a 30–50% chance of developing them. If both parents are allergic, the risk increases to around 70–80%. However, genetics alone do not determine allergy development. Environmental factors—including mode of delivery (vaginal vs. cesarean), early feeding practices, exposure to pets, and use of antibiotics—can influence the trajectory of a baby’s immune development. For example, research shows that vaginally delivered infants exposed to maternal vaginal flora may have more robust microbiomes, potentially reducing the risk of allergies.
Newborn allergies may also be influenced by maternal health during pregnancy. Inflammatory conditions, infections, or maternal diets high in ultra-processed foods may predispose infants to early sensitivities. This helps explain why even within the same family, some siblings develop allergies while others do not. Understanding the complexity behind do newborns get allergies helps dispel the myth that allergic conditions are purely hereditary or strictly the result of food exposure. Instead, a wide array of influences must be considered, often requiring a multidisciplinary approach to diagnosis and management.
Can a 5 Month Old Have Allergies? What to Expect at This Stage
Parents often wonder, can a 5 month old have allergies, especially as their baby becomes more interactive and begins exploring new foods and environments. The answer is yes—five months is a prime time for allergic symptoms to emerge, especially as solids may be introduced around this age. Even though exclusive breastfeeding is still common at five months, some infants are already reacting to environmental triggers like pet dander, pollen, or mold. At the same time, if a baby begins consuming cereals, fruits, or purees, the risk of food-related reactions increases, especially if those foods contain common allergens like eggs, wheat, or nuts.
At this stage, it is vital to differentiate between developmental changes and genuine signs of allergy. Increased drooling, teething discomfort, or inconsistent sleep may mimic the irritability caused by allergies. However, the appearance of hives, vomiting after feeding, or a baby food allergy rash that coincides with the introduction of new foods warrants careful evaluation. A pediatrician may suggest food elimination trials, skin prick tests, or referral to an allergist. This period is also an excellent time to educate caregivers about the importance of reading food labels, observing feeding responses, and maintaining a symptom diary to help pinpoint patterns that suggest sensitivity or intolerance.
What Does a Food Allergy Look Like in an Infant and How Is It Diagnosed?
Visual signs of infant food allergies often begin on the skin and may resemble common conditions like heat rash, eczema, or cradle cap. However, the hallmark of an infant allergic reaction to food is its consistency in relation to feeding and its recurrence upon re-exposure to the suspected allergen. A classic newborn food allergy rash tends to be red, inflamed, and may spread beyond the immediate area of contact. In more severe cases, angioedema—or swelling of the face, lips, or eyelids—can occur, requiring immediate medical attention. Gastrointestinal symptoms, such as vomiting, diarrhea, or excessive gas, are also common markers of an allergy-related reaction in babies.
Diagnosis typically involves a comprehensive history, including a review of feeding practices, family history of allergies, and symptom timing. In some cases, a pediatrician may perform specific blood tests to measure immunoglobulin E (IgE) levels, or refer the infant for skin testing with an allergist. These tests can identify antibodies specific to common allergens and help clarify whether the reaction is IgE-mediated (immediate onset) or non-IgE-mediated (delayed). This distinction is important because treatment strategies differ based on the underlying mechanism. Understanding what does a food allergy look like in an infant helps parents respond appropriately and reinforces the need for timely medical evaluation and intervention.

How to Introduce Allergens to Baby Safely and Strategically
Navigating the introduction of potential allergens to a baby’s diet can feel daunting, especially for families with a history of allergic conditions. However, emerging research strongly supports the idea that early introduction of allergens—particularly peanuts and eggs—can reduce the risk of developing allergies later in life. To introduce allergens to baby safely, parents are encouraged to wait until the infant is developmentally ready for solids, typically around six months, and to start with small, controlled portions. The baby should be healthy on the day of introduction and observed closely for at least two hours afterward for any signs of an allergic reaction.
For the best outcomes, allergens should be introduced one at a time, ideally under the guidance of a pediatrician if there is a known risk of allergy. Parents should understand how to tell if their baby is allergic to food by looking for consistent patterns of reaction, such as skin changes, vomiting, or behavioral shifts. In some cases, a proactive approach involving early introduction may be combined with allergy testing, especially if there has been a prior reaction or a sibling with severe allergies. By approaching this stage strategically, families can support tolerance development and potentially reduce the likelihood of future allergies.
Understanding Newborn Allergy Symptoms in the Context of Food and Environment
Recognizing newborn allergy symptoms is a skill that involves both scientific understanding and parental intuition. Symptoms may include a range of physical manifestations such as hives, persistent eczema, respiratory issues, and gastrointestinal distress. However, subtle signs—like inconsolable crying after feeding, prolonged sleep disruption, or changes in stool patterns—may also point toward an allergy, even if they are less specific. The challenge lies in connecting these symptoms with potential triggers, whether food-based or environmental. A child exposed to dust mites, pet dander, or mold may display symptoms that overlap with food-related allergies, complicating the diagnostic process.
To manage this complexity, clinicians often recommend a stepwise approach that starts with identifying the most likely allergens, adjusting feeding practices, and assessing the baby’s environment. This process can be time-consuming but is essential to prevent ongoing discomfort and the development of more serious allergic conditions. Parents should not attempt to self-diagnose or drastically alter feeding without professional input, as doing so can lead to nutritional deficiencies or missed diagnoses. In the end, understanding whether do newborns get allergies—and what those symptoms look like—requires patience, careful documentation, and collaboration with trusted healthcare professionals.
Key Takeaways on Baby Allergies, Skin Conditions, and Nutritional Strategies for Prevention
Caring for an infant who may be experiencing allergic reactions can be emotionally taxing and logistically complex, but gaining a deep understanding of the signs, triggers, and appropriate responses makes all the difference. The evidence is clear that yes, do newborns get allergies—and these early responses can present through the skin, gastrointestinal system, or respiratory tract. Recognizing the difference between typical infant behavior and signs of allergic sensitivity enables parents and caregivers to seek timely medical guidance and initiate effective interventions.
As families navigate the challenging journey of infant feeding and environmental exposures, strategies rooted in scientific evidence—such as early allergen introduction, observation of symptom patterns, and individualized nutritional guidance—offer a roadmap to better health outcomes. The presence of baby allergies, especially when marked by recurrent infant skin rash food allergy symptoms or gastrointestinal distress, should never be dismissed as routine. Instead, these signs may serve as important clues that a child’s immune system is reacting to a stimulus that warrants further exploration.
Informed parents can play a critical role in advocating for their baby’s health by partnering with pediatricians, staying updated on allergy prevention research, and adopting mindful feeding practices. Ultimately, the journey to understanding whether and how newborns have allergies is one of curiosity, vigilance, and compassion—anchored in the shared goal of ensuring that every child gets the healthiest start possible in life.
Frequently Asked Questions About Infant Allergies and Skin Conditions
Do Newborns Get Allergies from Their Environment or Feeding Practices?
Yes, newborns can develop allergic responses influenced by both their environment and what they consume—whether through breast milk, formula, or early solid foods. While the immune system is still immature, it is already forming critical responses based on exposure to common allergens like cow’s milk protein, dust mites, or even pollen. Environmental allergens often affect the respiratory tract or skin, while dietary proteins may trigger gastrointestinal or systemic symptoms. In some cases, even trace amounts of allergens passed through breast milk can sensitize an allergy infant. Understanding how immune memory is shaped early on is crucial; frequent exposure to allergens through skin contact, feeding, or airborne particles may contribute to the development of baby allergies over time.
What Does a Baby Food Allergy Rash Look Like Compared to Other Common Rashes?
A baby food allergy rash is often red, raised, and appears shortly after the introduction of a specific food. It commonly presents as hives or itchy patches that may spread across the cheeks, arms, or torso. Unlike heat rashes or cradle cap, which tend to be localized and less reactive, an infant food allergy rash is dynamic—it can appear suddenly and may worsen with re-exposure to the same food. It’s essential to distinguish between irritant rashes and true allergic responses; irritant reactions tend to be mild and resolve quickly, while an infant skin rash food allergy may persist, recur, or escalate. Consulting with a pediatric allergist can provide diagnostic clarity, especially when symptoms overlap with other infant skin conditions.
How Do Newborn Allergy Symptoms Differ from Colic or Normal Fussiness?
Newborn allergy symptoms often mimic typical infant behaviors such as colic, reflux, or sleep disturbances, making diagnosis challenging. However, consistent patterns—such as a baby developing a rash, diarrhea, or vomiting shortly after feeding—can suggest a deeper issue. While colic usually occurs in the late afternoon or evening and isn’t linked to specific foods, a newborn food allergy often causes prolonged crying after meals, visible discomfort, or refusal to feed. Parents should also watch for chronic nasal congestion, frequent sneezing, or breathing irregularities, which may indicate that can newborns have allergies to airborne particles or milk proteins. Documenting when symptoms occur in relation to meals or environmental changes can help differentiate between benign fussiness and food allergies in babies.
Do Newborns Get Allergies More Often If Their Parents Have Allergies?
Yes, genetics play a significant role in determining whether do newborns get allergies. If one parent has an allergic condition such as asthma, eczema, or food allergies, the baby has a higher risk of developing similar issues. When both parents have a history of allergies, that risk may increase substantially. However, not all children of allergic parents will develop allergic responses—environmental factors and early dietary exposures also matter. Emerging evidence suggests that the timing of allergen introduction and the diversity of a baby’s microbiome can influence outcomes in infants and food allergies. Preventive strategies like early peanut introduction, varied diets for breastfeeding mothers, and microbiome support are being explored to counteract genetic susceptibility.
Can a 5 Month Old Have Allergies Even Before Starting Solids?
Absolutely—can a 5 month old have allergies is a valid and medically recognized question. Many infants at this age may show allergic symptoms even before the introduction of solid foods, especially if they’re reacting to proteins in breast milk or formula. For instance, dairy or soy proteins consumed by a breastfeeding mother can pass through her milk and trigger a reaction in her infant. Formula-fed babies may develop sensitivities to cow’s milk or soy-based formulas. Symptoms in this age group often include infant food allergy symptoms like projectile vomiting, excessive gas, mucousy stools, or skin rashes. Because the immune system is still maturing, these responses may not be immediate, making symptom tracking critical during this phase.
How to Tell If Your Infant Has Allergies Without Formal Testing?
While formal allergy testing is valuable, there are observational methods that can offer preliminary insights into how to tell if your infant has allergies. Parents should monitor their baby’s reactions to feedings, especially when introducing new foods or switching formulas. Recurrent rashes, diarrhea, vomiting, nasal congestion, or changes in behavior like unusual irritability can all point to a potential allergy infant scenario. One effective strategy is keeping a detailed symptom diary, noting the time of feeding, ingredients, and any physical or behavioral changes. This record becomes a crucial diagnostic tool for pediatricians. In some cases, an elimination diet guided by a healthcare provider can offer strong evidence before more invasive tests are pursued.
What Does a Food Allergy Look Like in an Infant During an Emergency?
Severe food allergies in babies, though rare, can lead to life-threatening conditions like anaphylaxis. Knowing what does a food allergy look like in an infant during such events is critical. Signs may include rapid swelling of the face or lips, difficulty breathing, wheezing, or sudden lethargy. A bluish tint around the mouth, uncontrollable crying, or a widespread hivelike baby food allergy rash may also appear. Immediate emergency care is essential in these cases, and epinephrine may be administered by a healthcare provider if needed. Parents of infants and food allergies often carry an emergency action plan, especially if previous reactions were severe or involved multiple systems of the body.
How to Introduce Allergens to Baby Without Causing a Reaction?
Introducing allergens safely involves more than simply choosing the right food—it requires timing, portion control, and close monitoring. Pediatric experts recommend that once a baby shows readiness for solids, common allergens like peanuts, eggs, and fish should be introduced early and gradually. Parents wondering how to introduce allergens to baby should start with a small amount of the new food, ensure no other new foods are introduced simultaneously, and observe the baby for at least two hours post-feeding. If the baby tolerates the allergen well, it should be included regularly in the diet to build and maintain tolerance. Families with a history of allergy infant concerns may consider pre-testing or introducing high-risk foods in a clinical setting under supervision.
Can Infants Get Allergies from Skin Contact Rather Than Food Alone?
Yes, research increasingly shows that can infants get allergies through skin contact is a possibility, especially when the skin barrier is compromised due to eczema or other conditions. For example, exposure to peanut proteins through broken or inflamed skin may sensitize an infant before they ever ingest the food, a phenomenon supported by recent studies in pediatric allergy research. This highlights the importance of maintaining healthy, moisturized skin, particularly in infants with atopic dermatitis. Parents should be mindful of what comes into contact with their baby’s skin—this includes lotions, food residues on caregivers’ hands, and household dust. Protecting the skin barrier is now seen as a key strategy in reducing the risk of sensitization and future baby allergies.
Do Infants Have Allergies That Resolve Over Time, or Are They Permanent?
Many infant allergies are temporary and can be outgrown with time. For example, a newborn allergy to cow’s milk may resolve by the time the child reaches one to three years of age. However, other allergies—particularly those involving nuts, shellfish, or eggs—can be more persistent. The question of do infants have allergies that resolve or endure depends on several variables, including the type of allergen, severity of the initial reaction, and whether the immune system develops tolerance. Ongoing monitoring, repeat testing, and allergist consultations can help determine whether reintroduction is safe. Parents should never attempt food reintroduction without medical oversight, especially if the infant has experienced a prior infant allergic reaction to food or had concerning newborn allergy symptoms.
Bonus Insight: Do Newborns Get Allergies Differently Than Older Infants?
Yes, the way do newborns get allergies differs from how older infants experience them, largely due to developmental changes in the immune system and digestive tract. Newborns are more likely to exhibit generalized symptoms such as fussiness, vomiting, or failure to thrive, rather than clear-cut hives or wheezing. Because their immune system is still “learning” which substances are harmful versus harmless, allergic responses may be more subtle or delayed. In contrast, older infants who have begun solids or have more environmental exposure may show localized or immediate symptoms like an infant food allergy rash. Recognizing these differences is essential for timely diagnosis and the development of effective prevention strategies across the first year of life.
Conclusion: How to Tell If Your Infant Has Allergies and What It Means for Long-Term Health
As we reach the end of this in-depth exploration into newborn skin conditions and allergic reactions, one truth becomes increasingly clear: understanding how to tell if your infant has allergies is not only possible—it is essential for fostering long-term health and wellness. From early food sensitivities to visible signs like infant food allergy rash and eczema, the markers of allergy in infancy are varied but decipherable when parents and caregivers are equipped with the right knowledge. The question “do newborns get allergies” is no longer rhetorical; it is a clinically valid concern that deserves careful observation, informed response, and proactive nutritional planning.
Throughout the early stages of life, the immune system is in a state of rapid learning, influenced by genetics, environmental exposures, and dietary inputs. Knowing when to act and how to interpret symptoms—whether it’s recognizing newborn allergy symptoms or understanding what a food allergy looks like in an infant—can help prevent both short-term discomfort and long-term complications. Feeding strategies such as early, structured allergen introduction and the careful selection of breast milk or formula play a crucial role in shaping the infant’s immunological landscape. For many families, identifying infant food allergy symptoms and intervening early could mean reducing the risk of future conditions like asthma or eczema.
Moreover, integrating expert insights about baby allergies and skin manifestations into day-to-day parenting choices empowers families to make informed decisions rooted in science rather than fear. Whether you are monitoring a newborn food allergy rash, exploring how to introduce allergens to baby safely, or trying to determine if can infants have allergies to something in their environment, your attentiveness matters. Partnering with a knowledgeable pediatrician or allergist ensures that symptoms are evaluated in context, not in isolation, and allows for a tailored approach to care.
Ultimately, the journey of raising a healthy child starts with awareness—of signs, triggers, and the science that connects them. With thoughtful attention to both nutrition and early symptoms, parents can help their babies thrive while minimizing the burden of allergic disease. Understanding that do newborns get allergies is not just a theoretical question, but a practical concern rooted in immunological science, is a powerful first step toward lifelong wellness.
Further Reading:
GROWTH CLONE*What to do if a baby has an allergic skin reaction