Allergies are often dismissed as minor inconveniences, but for families managing life-threatening food allergies, the stakes are infinitely higher. One of the most pressing and terrifying questions a parent might ask is, can I die in sleep from anaphylaxis? This concern becomes even more urgent when it pertains to children, especially those who are too young to articulate symptoms or recognize danger. The possibility of fatal allergic reactions occurring during sleep is real, albeit rare, and it underscores the critical need for awareness, prevention, and emergency readiness. Understanding how to identify, respond to, and prepare for anaphylaxis is not only lifesaving—it is an essential act of advocacy and love for any parent raising a child with food allergies.
The science behind anaphylaxis reveals a complex and rapid physiological cascade. It is not just a severe allergic reaction; it is a full-body immune system response that can shut down airways, plummet blood pressure, and cause unconsciousness within minutes. What makes nocturnal anaphylaxis particularly insidious is the reduced likelihood of recognizing early symptoms during sleep, delaying life-saving intervention. This alone emphasizes the importance of knowing the 4 stages of anaphylaxis and how to prepare for each one. For families managing allergies to common foods such as peanuts, tree nuts, milk, eggs, and shellfish, understanding the difference between a routine allergic response and anaphylactic shock is crucial.
Moreover, there are important distinctions between anaphylaxis vs allergy. While many children outgrow milder allergies or manage symptoms with antihistamines, anaphylaxis is a different beast entirely. It demands fast-acting treatment, such as intramuscular epinephrine, and a comprehensive emergency plan. This article will guide you through every angle of this critical topic—from risk identification and symptom recognition to medical treatment for anaphylaxis and long-term prevention strategies tailored for children. Let’s delve into what every parent must know, not only to ask informed questions like “can I die in sleep from anaphylaxis,” but to confidently prevent and respond to such a terrifying possibility.
You may also like: Essential Facts About Baby Skin Conditions: Do Newborns Get Allergies and How to Tell
Understanding Anaphylaxis: What Every Parent Needs to Know
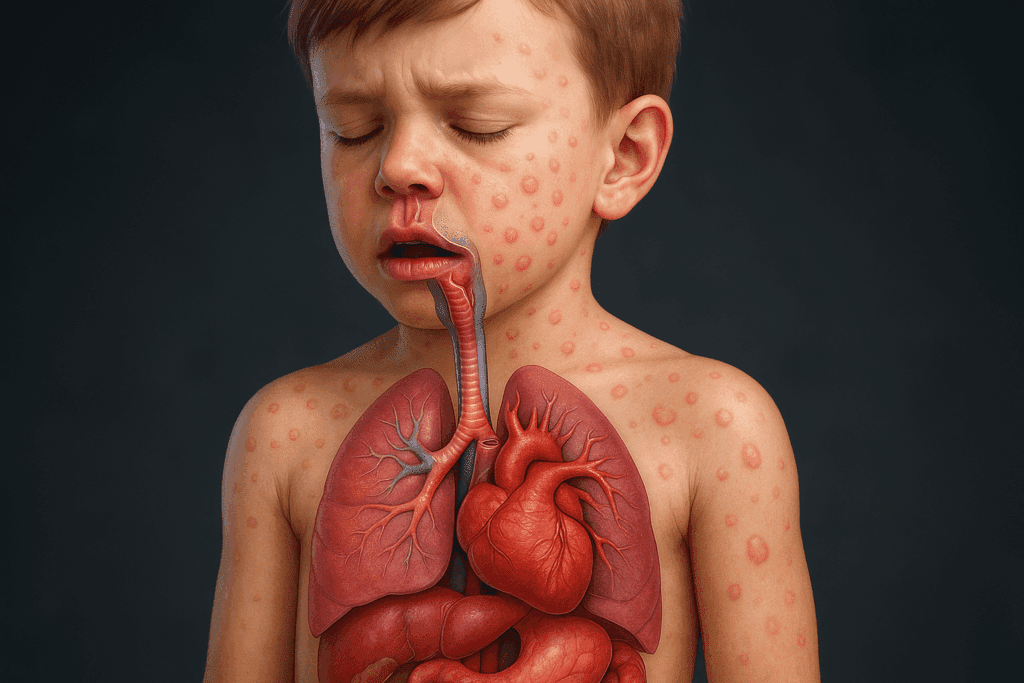
At its core, anaphylaxis is an overreaction of the immune system that can rapidly become life-threatening. Unlike common allergies, which may cause discomfort through hives, nasal congestion, or mild stomach upset, anaphylaxis involves a sudden release of chemicals like histamines that disrupt multiple organ systems. This reaction can trigger bronchoconstriction, cause the throat to swell shut, induce a dangerous drop in blood pressure, and lead to loss of consciousness. The onset is often sudden, though it can be preceded by mild symptoms that escalate within minutes. Understanding the 4 stages of anaphylaxis helps families detect the earliest signs and intervene before the reaction becomes unmanageable.
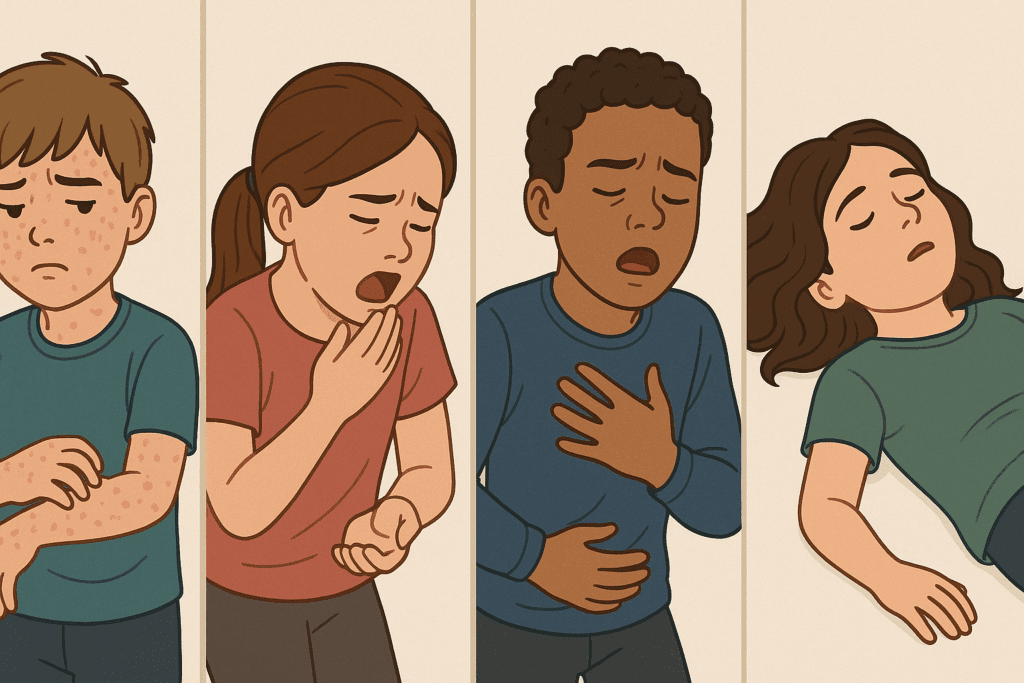
The initial stage typically involves symptoms like itching, hives, or swelling, often around the lips or face. This is followed by respiratory distress, where the child may wheeze, cough, or struggle to breathe. As the reaction intensifies, gastrointestinal symptoms such as vomiting or diarrhea may occur. The final and most critical stage is cardiovascular collapse, which manifests as dizziness, fainting, or shock. Recognizing the progression is crucial, especially in young children who may not be able to describe what they’re experiencing. Parents must be attuned to non-verbal cues like sudden lethargy, drooling due to throat swelling, or unusual behavioral changes during meals.
The 5 stages of allergic reaction provide a slightly more granular framework, breaking the process down into allergen exposure, immune system sensitization, histamine release, inflammation, and resolution or escalation into anaphylaxis. These frameworks aren’t mutually exclusive but help parents differentiate between transient symptoms and those requiring immediate emergency action. The stakes of understanding this distinction cannot be overstated, particularly when a child is sleeping and unable to alert others to what they’re experiencing. Monitoring tools, such as wearable medical alert devices or baby monitors with audio and video, can provide an added layer of surveillance for families managing high-risk allergies.
Can I Die in Sleep from Anaphylaxis? The Hidden Risks Parents Must Understand
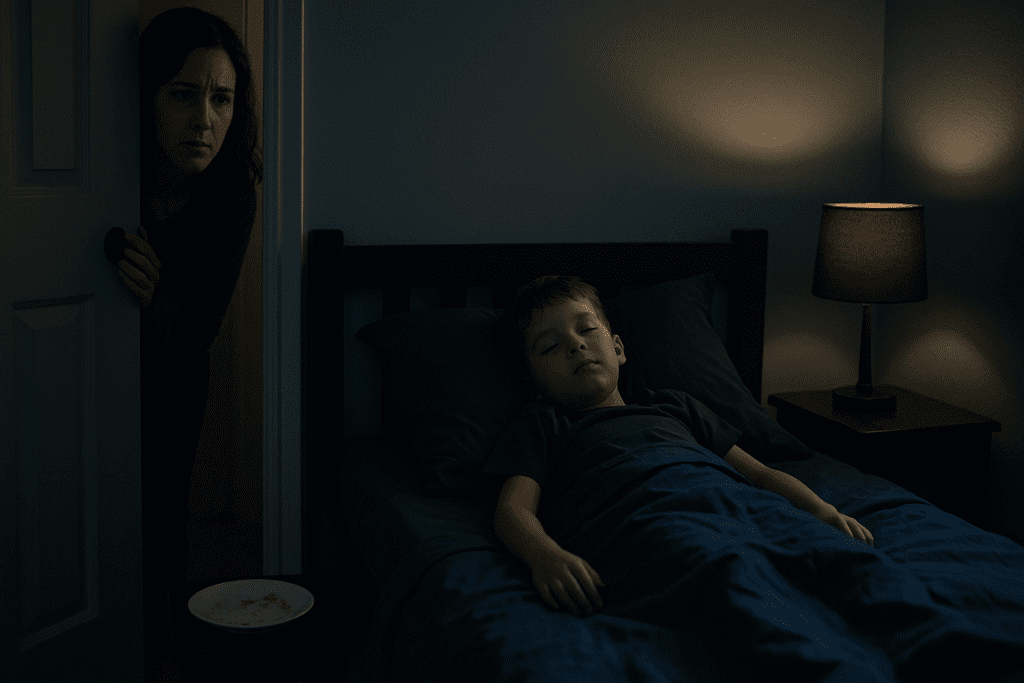
The question “can I die in sleep from anaphylaxis” is not merely theoretical—it is rooted in medical reality. While rare, nocturnal anaphylaxis is a documented phenomenon, and the outcomes can be devastating if the response is delayed or absent. This is especially concerning in households with young children who cannot articulate their symptoms or wake others for help. Deaths related to sleep-time anaphylaxis typically occur when early warning signs—like mild hives, a scratchy throat, or nasal congestion—go unnoticed and untreated, progressing to full anaphylactic shock during the night.
A key issue is that the body’s natural sleep processes can mask or mimic early symptoms of an allergic reaction. For instance, a child with mild nasal congestion or sleep-induced breathing irregularities may be mistakenly thought to be snoring or sleeping restlessly, when in fact, they are experiencing early-stage airway inflammation. Because anaphylaxis can progress in minutes, delayed recognition can have fatal consequences. Furthermore, lying flat may exacerbate symptoms by allowing swelling in the airway or lungs to worsen, which is particularly dangerous for children.
Recent case studies have reported fatal allergic reactions to common bedtime exposures, such as ingesting milk in evening snacks or reacting to allergens in bedding materials. These situations reinforce the importance of controlling the child’s environment and implementing strict allergen avoidance strategies, especially before bedtime. For families wondering if the use of antihistamines at night can prevent such outcomes, it’s important to clarify that while antihistamines may reduce mild allergic symptoms, they are not a substitute for anaphylaxis treatment. Only epinephrine is proven to reverse the physiological changes caused by severe allergic reactions.
This is why understanding the stages of allergic reaction and knowing how quickly anaphylaxis can strike—even in the absence of previous severe reactions—is critical for all caregivers. It’s also worth noting that delayed anaphylaxis can occur several hours after allergen exposure, meaning a child who appears fine after dinner could experience a reaction in the early morning hours. The gravity of this issue makes the presence of emergency medications like auto-injectable epinephrine a non-negotiable in homes with at-risk children. The reassurance that comes from being prepared can transform parental anxiety into empowered action.
Recognizing the Stages of Allergic Reaction in Children
Understanding the stages of allergic reaction is one of the most effective tools parents have for protecting their children. At the earliest stage, children may experience minor skin reactions such as hives, itchiness, or redness. These symptoms are often mistaken for mosquito bites, rashes, or even dry skin, particularly in infants and toddlers. However, their presence following food intake should raise immediate red flags. These signs are not to be ignored, even if they resolve spontaneously, as they may indicate that the child’s immune system has been sensitized to a specific allergen, placing them at risk for future anaphylaxis.
As the immune system mounts a stronger response, gastrointestinal symptoms may occur, including vomiting, diarrhea, or abdominal cramps. This stage often coincides with histamine release and inflammation, which can escalate depending on the allergen dose and the child’s immune sensitivity. Respiratory symptoms such as coughing, wheezing, or throat tightness typically follow and should always be treated as medical emergencies, even in the absence of hives or gastrointestinal distress. By the time cardiovascular symptoms—like pallor, clamminess, or unconsciousness—emerge, the child is likely experiencing anaphylactic shock.
Parents who understand these stages are better equipped to make rapid, life-saving decisions. Familiarity with the 5 stages of allergic reaction can inform treatment strategies and improve communication with healthcare providers. For instance, noting the exact timeline and types of symptoms that appeared before intervention can help allergists identify the specific triggers and assess risk for future episodes. Education also plays a key role in community preparedness—knowing when to call emergency services, how to administer an epinephrine auto-injector, and when to administer antihistamines can significantly alter the outcome of an allergic episode.
Anaphylaxis vs Allergy: Why the Difference Matters in Emergency Scenarios
Differentiating between anaphylaxis vs allergy is not merely a matter of semantics—it can be the difference between a proactive response and a fatal delay. Allergies often present with localized symptoms like sneezing, watery eyes, or mild rashes. These reactions, while uncomfortable, typically resolve without systemic involvement and are managed with oral antihistamines or topical creams. In contrast, anaphylaxis is a systemic and rapidly progressive condition that involves multiple organ systems and requires urgent medical intervention.
The confusion often arises because mild allergic reactions can precede anaphylaxis, especially in children who have had prior exposures without major symptoms. For example, a child who previously developed a minor rash from eating peanuts may later experience a full-blown anaphylactic response upon re-exposure. This unpredictability emphasizes the need for parents to treat every allergic episode seriously and to have an action plan in place. The presence of even one symptom involving the respiratory or cardiovascular system—no matter how mild—should trigger immediate use of an epinephrine auto-injector.
Furthermore, the distinction affects treatment protocols. While antihistamines may alleviate hives or itching, they do not prevent airway closure or cardiovascular collapse. Only epinephrine halts the physiological spiral of anaphylaxis by constricting blood vessels, opening airways, and stabilizing blood pressure. This is why understanding the difference between allergies and anaphylaxis is so vital, particularly when symptoms occur during sleep or when the child is alone. In such cases, fast-acting intervention can literally mean the difference between life and death.
Medical Treatment for Anaphylaxis: What Every Parent Should Keep On Hand
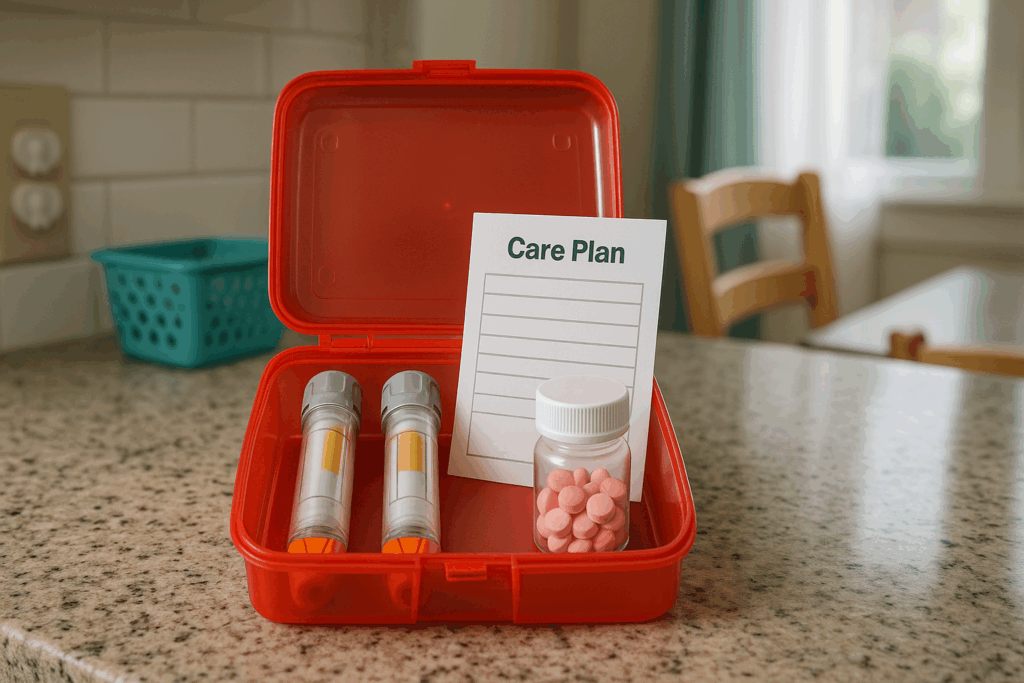
When it comes to treating anaphylaxis, speed is everything. The first and most critical intervention is intramuscular epinephrine, which works within minutes to reverse airway swelling, stabilize circulation, and halt the immune system’s escalating response. Parents should always have at least two epinephrine auto-injectors available, as a single dose may not be sufficient, particularly if emergency medical services are delayed. This is not an area for compromise—having unexpired, properly stored medication readily accessible at all times is a non-negotiable safety measure.
Beyond epinephrine, the next step in anaphylaxis treatment often involves supportive care from medical professionals. This includes oxygen administration, intravenous fluids, antihistamines, and corticosteroids. These treatments help stabilize the child and prevent biphasic anaphylaxis—a delayed recurrence of symptoms that can occur hours after the initial episode. Therefore, even after administering epinephrine, immediate medical attention is mandatory. Parents should never assume that symptoms have resolved or that no further care is needed simply because their child appears to improve.
In addition, families should consider medical alert identification for children, such as bracelets or tags, which can inform bystanders and emergency personnel of the child’s allergies in case the caregiver is not present. Schools, babysitters, and extracurricular programs should all be provided with written emergency action plans, including instructions for treating anaphylaxis. Training family members and caregivers on how to recognize symptoms and administer epinephrine is equally crucial. No parent can predict every risk, but having a robust response strategy ensures they are never unprepared.
Can I Die in Sleep from Anaphylaxis? How to Minimize Nighttime Risks for Children
The haunting question—can I die in sleep from anaphylaxis—carries even greater emotional weight for parents of children with food allergies. The thought that a child might quietly slip into a life-threatening allergic reaction during the most vulnerable hours of the night is terrifying. Fortunately, there are proactive steps parents can take to drastically minimize this risk. The first and most effective strategy is strict allergen avoidance, particularly in the hours before bedtime. This includes eliminating known allergens from dinners and evening snacks, double-checking ingredients, and preventing cross-contact in kitchen tools and surfaces. It also means being extra vigilant when children are away from home, such as during sleepovers, school events, or vacations.
Additionally, parents should remain cautious of hidden allergens in toothpaste, medications, or even soaps and lotions that might be used at night. For example, some topical products may contain milk proteins or nut oils, which can cause a reaction in highly sensitive children. Ensuring the bedroom environment is free of allergens—like feather bedding, dust mites, or pet dander—is also crucial. In some cases, environmental triggers like mold spores or pollen may exacerbate underlying allergic responses that, when combined with dietary allergens, push the immune system over the edge.
It’s important to use technology wisely. For young children, especially those under five, using a high-quality baby monitor with sound and video capabilities allows parents to hear unusual breathing or see changes in sleep posture that may indicate distress. For older children, wearable devices that detect heart rate or oxygen saturation may provide another layer of security, although they are not substitutes for clinical monitoring. In cases where the child has a history of severe, nocturnal reactions, a shared sleeping space may be temporarily considered for enhanced monitoring. Open communication with pediatricians and allergists can help refine these strategies and determine when such measures are appropriate.
Ultimately, education and preparedness are the greatest shields against the tragic possibility of nocturnal anaphylaxis. Children who are old enough should be taught to identify their symptoms and call for help, even in the middle of the night. Teaching them not to ignore hives, throat itchiness, or unusual tiredness—even if it interrupts their sleep—can empower them to protect themselves. With a layered approach combining environmental control, strategic timing of food consumption, and medical readiness, the risk of death during sleep from anaphylaxis becomes not only manageable but significantly reduced.
Treating Anaphylaxis at Home: Emergency Action Plans for Parents
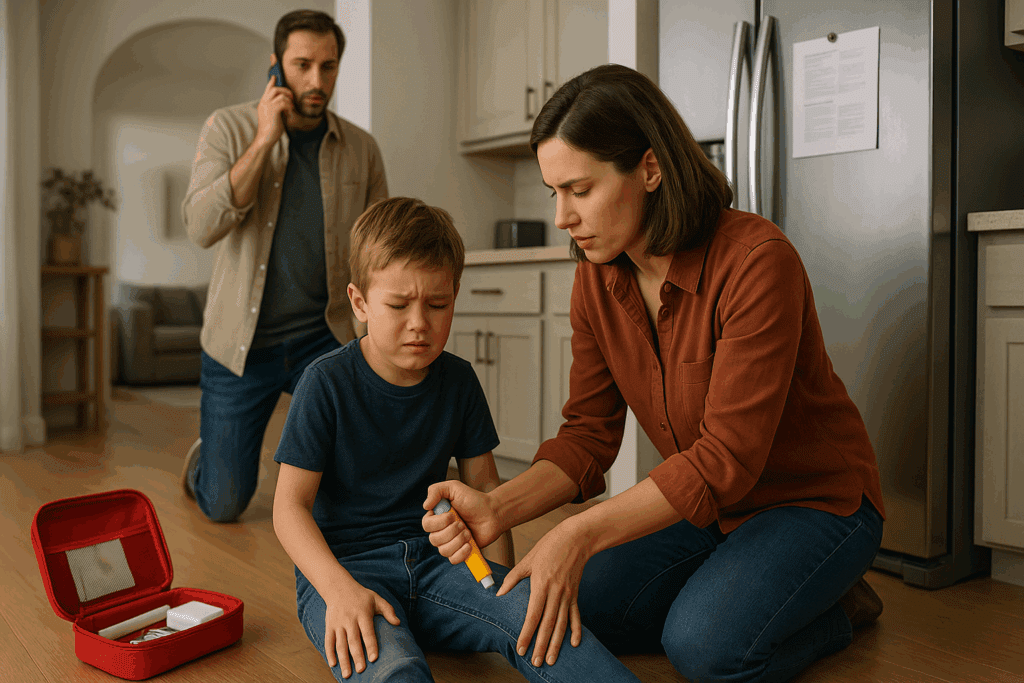
Creating an emergency action plan is not just a recommendation—it’s a foundational component of responsible allergy management. When it comes to treating anaphylaxis, the first few minutes are critical. At the core of the plan should be the immediate use of epinephrine at the first sign of a severe reaction. Parents must be trained to recognize these signs, including difficulty breathing, swelling of the face or throat, sudden hives, wheezing, or loss of consciousness. While it’s tempting to “wait and see,” any delay can result in irreversible consequences.
Each plan should also clearly identify when to call emergency services. The moment epinephrine is administered, 911 should be called to ensure the child receives ongoing medical treatment. This is crucial because of the possibility of biphasic reactions, where symptoms return hours after initial improvement. Having written instructions, often provided by the child’s allergist, can ensure that caregivers, teachers, and even older children themselves understand the necessary steps. These documents should be accessible—posted on the fridge, carried in the child’s backpack, and shared with anyone responsible for the child’s care.
The emergency kit itself should include not only two epinephrine auto-injectors but also an oral antihistamine and, when advised by a healthcare provider, a corticosteroid for secondary symptoms. However, it’s vital to remember that antihistamines and steroids are supportive—they are not substitutes for epinephrine in the treatment of anaphylaxis. Every six months, parents should check the expiration dates of all medications and review the action plan with their child’s care team. Additionally, parents should advocate for training sessions at schools or childcare centers so that staff are confident in administering epinephrine and recognizing the progression of symptoms.
Equally important is debriefing after an incident. Following a reaction, parents should document the timeline, symptoms, interventions used, and any factors that may have contributed to the exposure. This information can help allergists adjust the child’s management plan and further reduce risks. By treating the emergency plan as a living, evolving document, families can stay one step ahead of this unpredictable and dangerous condition.

Can I Die in Sleep from Anaphylaxis? How Food Allergies in Children Increase Risk
When food allergies are diagnosed in children, particularly in infancy or toddlerhood, the question can I die in sleep from anaphylaxis becomes a legitimate concern that must be addressed with compassion, knowledge, and strategy. Children are uniquely vulnerable because they often lack the language skills to describe symptoms and may not understand the urgency of a reaction. Even older children, despite being taught to speak up, might be embarrassed to call for help in the middle of the night, fearing it may be “just a rash” or “a tummy ache.” These communication barriers make nighttime reactions particularly hazardous.
Children with multiple food allergies or comorbid conditions such as asthma face an even higher risk. Asthma can complicate respiratory responses during anaphylaxis, making it more difficult to breathe and more likely for a reaction to escalate rapidly. Moreover, the presence of eczema or other allergic conditions often signals a more reactive immune system overall. In these cases, even trace amounts of allergen exposure can tip the balance. For instance, a child who touches a surface with peanut residue and later rubs their eyes or puts fingers in their mouth before bed might inadvertently set off a chain of events leading to a reaction while they sleep.
An additional risk factor comes from inconsistent allergy management practices. Some children outgrow certain allergies, but others do not, and assuming tolerance without confirmation through medically supervised food challenges can be dangerous. Parents should avoid interpreting a lack of recent reactions as evidence that an allergy has resolved. Testing and careful reintroduction should always be guided by an allergist. Similarly, children who have never had a severe reaction are still at risk; anaphylaxis can occur on the first known exposure or after a long history of mild reactions.
For parents and caregivers, acknowledging the reality of food allergy severity doesn’t mean living in constant fear. Rather, it means being informed, prepared, and vigilant. Consistent routines, strict avoidance, reliable medication access, and comprehensive education for everyone involved in the child’s life provide the protective framework necessary to ensure safety—even during sleep. The goal is not just survival, but thriving within healthy boundaries that respect the reality of the condition while preserving the joys of childhood.

Building Long-Term Strategies to Prevent Anaphylaxis in Growing Children
As children grow, so too must their allergy management strategies. Toddlers require close parental supervision, but as they become school-aged, the emphasis shifts toward education, independence, and community involvement. Parents must help children develop the skills to read food labels, recognize symptoms, and advocate for themselves. The earlier this process begins, the more second-nature it becomes. Schools play a central role in this transition, and parents should proactively engage with administrators, nurses, and teachers to develop individualized health care plans.
These plans should detail safe snacks, eating environments, and emergency protocols. Ideally, classroom activities involving food should be allergy-aware or allergen-free, especially in early grades. Children should be trained not to accept food from peers, and birthday treats should either be pre-approved or avoided. At lunch, assigned allergy-safe zones or tables can reduce the risk of cross-contact, although it’s essential to balance safety with inclusivity. Social isolation should never be the byproduct of allergy management.
Recreational activities and travel introduce additional variables. Whether it’s summer camp, sports teams, or family vacations, parents must scout ahead to ensure allergen-safe meals, trained staff, and emergency medication access. Medical treatment for anaphylaxis should be discussed with all caregivers in advance, including the location of auto-injectors and the specific steps to follow if a reaction occurs. At home, consider role-playing emergency scenarios so that children are confident and not paralyzed by fear during an actual event.
This proactive approach includes keeping pace with medical innovations. Advances in allergy desensitization therapy, including oral immunotherapy (OIT), are offering new hope for some families. While not suitable for everyone, these treatments aim to increase the child’s threshold to allergens under strict medical supervision. For some, they provide additional protection against accidental exposures, though they should not replace vigilance or emergency preparedness. The goal is to tailor the child’s allergy management as they age—revisiting their care plan regularly and making adjustments based on their developmental stage, medical updates, and environmental exposures.
Frequently Asked Questions: Essential Insights for Managing Anaphylaxis and Food Allergies in Children
What makes nighttime anaphylaxis particularly dangerous for children?
Nighttime anaphylaxis is especially perilous because early symptoms can go unnoticed as children sleep. The child may not recognize subtle signs such as a tightening throat, itching, or mild swelling, and even if they do, they may not wake up or call for help in time. During sleep, breathing patterns slow, which can mask early respiratory symptoms that might otherwise be caught while awake. This delay in recognition is one of the reasons why can I die in sleep from anaphylaxis is a valid concern for parents managing severe allergies. In addition to proactive bedtime routines and environmental allergen control, using wearable monitors that track respiration or oxygen levels may offer additional protection for children at higher risk.
How do the 4 stages of anaphylaxis inform emergency response planning?
Understanding the 4 stages of anaphylaxis—initial symptoms, respiratory involvement, gastrointestinal distress, and cardiovascular collapse—helps caregivers respond with greater precision and urgency. Early identification of the first stage, such as sudden hives or throat discomfort, allows for quicker intervention before the reaction progresses to more dangerous stages. Recognizing the sequential nature of these symptoms can also help caregivers differentiate between a mild allergic reaction and a true emergency. In practice, having this knowledge allows parents and caregivers to better time the use of epinephrine and avoid unnecessary delays. It also empowers families to provide clearer symptom timelines when communicating with emergency responders and allergists during follow-up care.
How do the 5 stages of allergic reaction help identify long-term allergy patterns?
The 5 stages of allergic reaction—exposure, sensitization, histamine release, inflammation, and resolution—reveal more than just acute episodes; they highlight broader patterns in allergic development. For instance, repeated exposure to small amounts of allergens over time can lead to sensitization, even if no severe symptoms are initially present. Parents might notice recurring mild symptoms—like eczema flare-ups or digestive issues—without realizing they signify a growing sensitivity that could escalate into full-blown anaphylaxis. Understanding these stages can prompt earlier allergy testing and intervention before a severe event occurs. This framework is especially helpful for pediatricians and allergists when developing individualized prevention plans for children showing multiple allergic tendencies.
What distinguishes effective anaphylactic shock treatment in clinical settings from at-home care?
In clinical settings, anaphylactic shock treatment goes beyond the initial epinephrine injection. Hospitals provide oxygen therapy, intravenous fluids, and continuous monitoring for cardiac and respiratory function. Unlike at-home care, which focuses on administering epinephrine and calling emergency services, hospitals can administer second-line medications like corticosteroids and H1 and H2 blockers to reduce inflammation and prevent a biphasic reaction. Advanced airway management, such as intubation, may also be necessary in extreme cases. Parents should understand that while treating anaphylaxis at home begins the life-saving process, full stabilization requires the clinical resources only emergency departments can offer.
How is anaphylaxis treatment evolving with new technologies and protocols?
Anaphylaxis treatment is advancing rapidly thanks to innovations in drug delivery systems and predictive allergy management. Newer epinephrine auto-injectors are being developed with digital tracking features that record injection times and alert caregivers to renew expired devices. Researchers are also exploring sublingual and intranasal epinephrine alternatives that may be easier for children to tolerate, especially those with needle phobia. Another emerging trend involves digital platforms that track allergen exposure risk based on location and environmental data, alerting families to heightened risk in real time. These innovations promise to enhance how treating anaphylaxis is approached, potentially reducing human error and improving response speed during emergencies.
What practical differences exist between anaphylaxis vs allergy in school settings?
In schools, the distinction between anaphylaxis vs allergy determines policies on medication storage, staff training, and meal planning. Children with mild allergies may be allowed to self-monitor or carry oral antihistamines, while those at risk for anaphylaxis typically require epinephrine auto-injectors stored in accessible, labeled locations. Teachers and staff often receive formal training in recognizing the signs of anaphylaxis and in administering medication, a protocol not typically followed for children with mild seasonal allergies or skin sensitivities. Cafeteria procedures, classroom food policies, and field trip planning also differ significantly depending on whether the child has a history of severe reactions. The need for individualized emergency care plans becomes more urgent and specific when managing children at risk of anaphylaxis.
Can I Die in Sleep from Anaphylaxis? How Allergy Thresholds Change Over Time
Many parents are surprised to learn that allergy thresholds can shift unpredictably, making the question can I die in sleep from anaphylaxis even more relevant as children grow. A child who previously tolerated trace exposures without incident may suddenly develop a heightened sensitivity due to immune system changes or cumulative exposures. Factors such as illness, asthma, hormonal changes, or even stress can influence immune reactivity. For example, a mild cold may increase vulnerability to allergens, making a nighttime exposure more likely to trigger an exaggerated response. Regular check-ins with an allergist and updated allergy testing are essential to monitor changes in threshold, especially during growth spurts, puberty, or after periods of allergen avoidance.
What are some emerging approaches to medical treatment for anaphylaxis in pediatric care?
New approaches to medical treatment for anaphylaxis in children include personalized allergy desensitization programs and immunomodulatory therapies. Oral immunotherapy (OIT), for example, involves the controlled administration of small amounts of the allergen under strict supervision, with the goal of increasing the child’s tolerance threshold. Biologic medications like omalizumab are being explored to help modulate the immune response in children with multiple allergies or asthma. Additionally, some pediatric programs are testing the use of wearable epinephrine devices that continuously monitor for early signs of anaphylaxis and automatically alert caregivers or emergency services. While still in development, these innovations show promise for expanding how anaphylaxis treatment is administered and improving safety in younger populations.
How do the stages of allergic reaction impact mental health in children with food allergies?
The stages of allergic reaction often come with intense physical symptoms that can cause psychological trauma, particularly in young children who may not fully understand what’s happening. Even when the reaction is resolved, the fear associated with the event can linger, sometimes manifesting as anxiety around eating, obsessive food checking, or avoidance of social events like birthday parties or school lunches. Children may internalize a sense of vulnerability or difference, which can affect self-esteem and peer relationships. Helping children process these experiences through counseling or support groups tailored for allergy sufferers is critical. Addressing the psychological impact is just as important as managing the physical stages of reaction, ensuring the child’s emotional resilience grows alongside their allergy management skills.
Can I Die in Sleep from Anaphylaxis? Building Emotional Resilience in Parents and Children
When facing the difficult reality posed by can I die in sleep from anaphylaxis, emotional preparedness is as vital as physical readiness. Parents often struggle with sleep disturbances, anxiety, or hypervigilance—especially after their child has had a severe reaction. Similarly, children may experience nightmares or sleep refusal due to fear of nighttime allergies. Mental health professionals recommend establishing calming routines, using positive language around allergy management, and focusing on empowerment rather than fear. Techniques such as cognitive behavioral therapy (CBT) have shown promise in helping both children and caregivers manage anticipatory anxiety and build confidence. Developing a resilient mindset doesn’t mean ignoring the risks—it means preparing for them while preserving emotional well-being and daily joy.
Conclusion: How Informed Allergy Management Protects Children from Anaphylaxis, Day and Night
The frightening possibility encapsulated in the question can I die in sleep from anaphylaxis is not meant to instill panic but to ignite preparedness and empower parents. The truth is that while the risk of fatal nocturnal reactions exists, it can be dramatically minimized through knowledge, preparation, and action. Understanding the 4 stages of anaphylaxis and the 5 stages of allergic reaction allows parents to decode the body’s early warning signs and act before a manageable reaction turns catastrophic. Knowing the difference between anaphylaxis vs allergy gives clarity to decisions made in the heat of the moment, and learning how to initiate anaphylaxis treatment—especially medical treatment for anaphylaxis with epinephrine—can save lives.
But knowledge alone isn’t enough. It must be translated into systems: emergency action plans, training for caregivers, school involvement, and developmentally appropriate education for children. These systems create a safety net that protects children not only during daylight hours but through the long night as well. With thoughtful prevention strategies and a solid understanding of treating anaphylaxis, families can shift from a reactive mindset to one of confident, proactive care. Parents become not just guardians but educators, advocates, and life-savers.
Ultimately, raising a child with food allergies is a long-term commitment that blends medical vigilance with everyday parenting. It’s about crafting a lifestyle that empowers children to navigate their world safely, even as they explore new environments, friendships, and milestones. With every label read, every meal plan double-checked, and every epinephrine refresher completed, parents build a wall of protection around their children. And in doing so, they answer the haunting question not with fear, but with unwavering readiness: Yes, the risk exists—but here, in this home, this school, this life, we are ready.
Further Reading:
Can You Die in Your Sleep from Anaphylaxis?
Anaphylaxis in Infants & Children: Responding to Severe Allergic Reactions



