Ensuring your newborn receives optimal nourishment from the very start is one of the most important responsibilities of new parenthood. While breastfeeding is a popular choice, millions of families around the world rely on bottle feeding to meet their baby’s nutritional needs. For many, understanding how to bottle feed a newborn becomes an essential skill—one that supports healthy growth, fosters bonding, and helps meet key developmental milestones. Whether you’re using expressed breast milk or formula, bottle feeding is both a practical solution and a nurturing opportunity that, when done correctly, can promote security, satiety, and strong parent-child connections.
You may also like: Essential Milestones in Baby Led Weaning: A Proven Guide to Nurturing Healthy Eating Habits
Why Bottle Feeding Matters in Early Infant Nutrition
Feeding is not just about filling a baby’s stomach—it’s about supporting every facet of their development. From the moment they’re born, newborns rely entirely on caregivers to deliver nutrients that are critical for brain development, physical growth, and immune system function. Bottle feeding can provide these needs reliably and flexibly, especially when breastfeeding is not possible, insufficient, or not preferred. Parents may turn to infant bottle feeding for a variety of reasons, including medical conditions, milk supply issues, work schedules, or personal choice. Regardless of the reason, the key is to ensure that the feeding method is safe, responsive, and nutritionally sound.
Bottle feeding also enables other caregivers to be involved in the feeding process, promoting shared responsibility and emotional bonding with both parents. Fathers, grandparents, or adoptive parents can participate fully in newborn care, creating a nurturing environment that encourages connection and trust. Moreover, feeding a baby by bottle offers the ability to measure intake precisely, which is reassuring for caregivers monitoring weight gain or feeding issues.

Understanding the Basics: Preparing for Infant Bottle Feeding Success
Before diving into the actual process of bottle feeding, it’s crucial to understand the tools, techniques, and hygiene standards required to support safe feeding practices. Bottle feeding success starts with proper preparation, including the selection of appropriate bottles, nipples, and formula or expressed breast milk.
Selecting the right bottle can be overwhelming given the wide variety of designs on the market. Some are anti-colic, some mimic the shape of a breast, and others are angled for ease of use. What matters most is choosing a bottle that works for your baby’s feeding style. Newborns often do best with slow-flow nipples, which prevent them from being overwhelmed by fast milk delivery. These nipples help babies pace themselves, mimicking the rhythm of breastfeeding and reducing the risk of overfeeding or digestive discomfort.
Proper hygiene is non-negotiable. Bottles and nipples must be sterilized before first use and washed thoroughly after every feed. This can be done using boiling water, steam sterilizers, or dishwashers with a sanitizing function. Clean hands and surfaces further reduce the risk of introducing bacteria that could harm a baby’s vulnerable digestive system. Formula preparation also demands precision: always follow the instructions on the packaging and use safe, filtered water to mix. Incorrectly prepared formula can lead to nutritional imbalances or dehydration.

How to Bottle Feed a Newborn: A Step-by-Step Approach to Nurturing Nutrition
Understanding how to bottle feed a newborn correctly involves more than just offering a bottle—it’s a holistic process that includes positioning, timing, responsiveness, and emotional presence. Begin by ensuring that your baby is calm, alert, and hungry—but not overly fussy. Feeding a distressed baby can be challenging and may lead to swallowed air or refusal of the bottle.
Hold your baby in a semi-upright position, cradled in your arms, with their head slightly elevated. This posture helps prevent ear infections, supports digestion, and allows for eye contact, which enhances bonding. Tilt the bottle so the nipple is always full of milk, minimizing the chance of air ingestion, which can contribute to gas and colic. Never prop a bottle or leave a baby unattended while feeding, as this can lead to choking and interferes with the emotional nurturing component of feeding.
Allow the baby to feed at their own pace. Watch for cues that they are hungry (rooting, sucking on fists) and signals that they are full (turning away, slowing sucking, or falling asleep). Responsive feeding—attending to these cues—supports healthy appetite regulation and reduces the risk of overfeeding. Burping your baby halfway through and after feeding is important, too, as it helps release any air swallowed during the process.
How to Bottle Feed a Newborn During the First Weeks of Life
In the first few weeks, learning how to bottle feed a newborn means adapting to their rapidly changing needs. Newborns have tiny stomachs and require frequent, small feedings—often every two to three hours, including throughout the night. Their nutritional requirements are high relative to their body size, and consistent, gentle feedings help them grow steadily while also reinforcing a sense of security.
At this stage, caregivers must also monitor signs that feeding is going well. These include steady weight gain, adequate wet and dirty diapers, and a content demeanor after feeding. If the baby seems excessively fussy, gassy, or is spitting up large amounts, this could indicate a problem with feeding technique, formula type, or bottle design. In such cases, it’s wise to consult with a pediatrician or lactation consultant who has experience with infant bottle feeding and can offer tailored advice.
During this period, it’s also helpful to keep a feeding journal. Track how much the baby eats, how often, and how they respond. Patterns will emerge that guide future feedings and may also highlight any issues that need medical attention. The more observant and flexible you are during these early weeks, the smoother the transition to longer stretches between feedings will be.

Supporting Healthy Growth with Bottle Feeding Techniques
When it comes to infant bottle feeding, the ultimate goal is to support healthy, steady growth. This includes more than just meeting caloric requirements—it also involves fostering positive feeding behaviors and laying the foundation for lifelong nutritional habits. Bottle-fed infants can thrive just as well as breastfed babies when care is taken to ensure appropriate feeding amounts and schedules.
One of the critical aspects of supporting growth is avoiding overfeeding. It’s easy to assume that a full bottle must be finished or to interpret every cry as hunger. However, this can lead to an excess intake, which has been associated with rapid weight gain and later obesity risk. Instead, honor your baby’s fullness cues and avoid pressuring them to finish a bottle. Let feeding be a time of comfort, not coercion.
Growth spurts are also common in the first year of life and can temporarily alter your baby’s feeding needs. You may notice increased hunger, more frequent waking at night, or restlessness. These are signs that your baby’s body is growing rapidly and requires more nourishment. Adjust bottle amounts gradually, and remember that these changes are often temporary. A baby’s appetite will naturally regulate itself again after the growth spurt subsides.
How to Bottle Feed a Newborn While Encouraging Emotional Bonding
Feeding is an intimate experience, and learning how to bottle feed a newborn in a way that promotes bonding is just as important as nutritional adequacy. Eye contact, touch, tone of voice, and presence all contribute to the emotional richness of feeding. Even if a baby is bottle-fed rather than breastfed, these nurturing aspects of the feeding experience remain just as powerful.
Try to hold your baby close during feedings, skin-to-skin when possible, and speak gently or sing softly. Let them hear your voice, feel your warmth, and sense your attention. These moments build trust, emotional security, and attachment—all foundational elements for healthy psychological development. Alternating who feeds the baby can also be a bonding opportunity for other caregivers, further enriching the infant’s social world.
Moreover, feeding time is a window into your baby’s emotional cues. Over time, you’ll learn to distinguish their hungry cry from their tired cry, their satisfied gaze from their overstimulated fussiness. This communication forms the foundation of responsive parenting and supports emotional intelligence, even from the earliest days of life.

Choosing the Right Formula for Bottle Feeding Success
For those not using expressed breast milk, selecting the right formula is a crucial step in mastering infant bottle feeding. There are many types of infant formula available, including cow’s milk-based, soy-based, hypoallergenic, and specialty formulas for reflux or allergies. The choice should be guided by your pediatrician, especially if your newborn has shown signs of intolerance, digestive discomfort, or family history of food allergies.
Most standard formulas are designed to closely mimic the nutrient profile of breast milk, though they cannot replicate its antibodies and live cells. That said, for the vast majority of babies, commercially available infant formulas are safe, nutritionally adequate, and regulated to meet strict safety standards. It is important to prepare and store formula correctly—never reuse leftover milk, avoid warming bottles in the microwave, and discard any unused formula after an hour.
Some parents experiment with different formulas due to issues like gas, colic, or spit-up. While it’s natural to want relief for your baby, it’s advisable to consult a pediatrician before switching formulas, as frequent changes can disrupt digestion further. Finding the right formula can take time, but when combined with appropriate feeding practices, most babies adapt well and thrive.
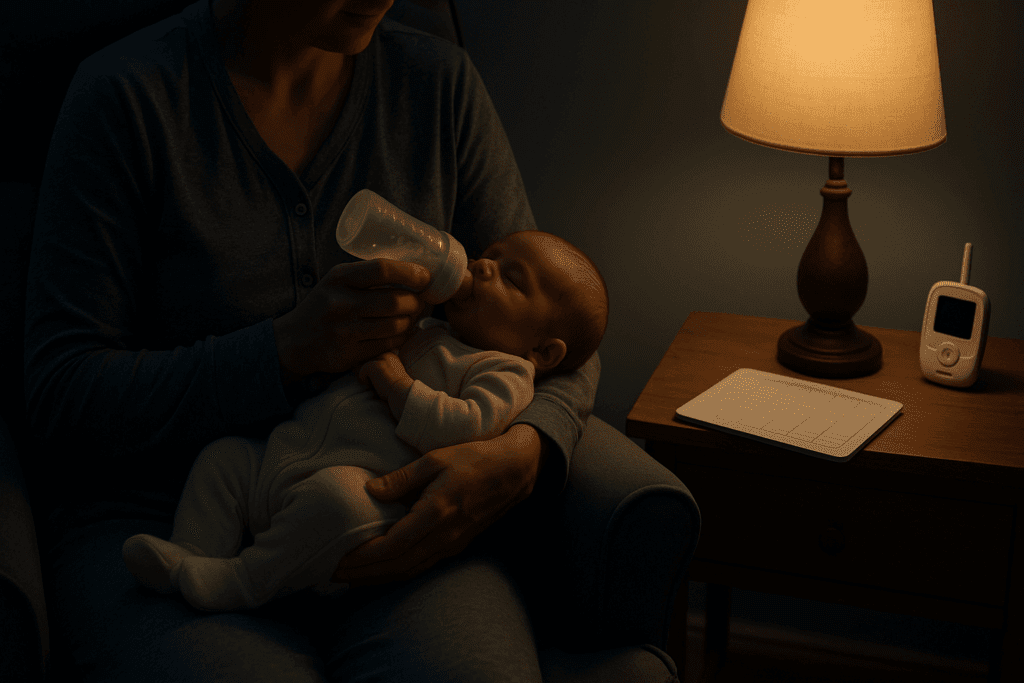
Nighttime Strategies: How to Bottle Feed a Newborn for Restful Sleep and Nutritional Consistency
Understanding how to bottle feed a newborn during the night is an essential part of maintaining a healthy feeding schedule and supporting uninterrupted growth. Newborns do not differentiate between night and day during their early weeks of life, so their nutritional demands persist around the clock. This means that caregivers must be prepared for frequent nighttime feeds, often every two to three hours. These night feeds provide not only essential calories but also help maintain hydration and stabilize blood sugar levels during the critical early months.
To make nighttime bottle feeding smoother, preparation is key. Keep bottles pre-sterilized and formula measured or breast milk thawed in advance. Consider setting up a small feeding station in your bedroom with everything you need within arm’s reach. Use dim lighting to avoid overstimulation, and speak softly to preserve a calming atmosphere that encourages your baby to return to sleep after feeding.
It’s also beneficial to keep nighttime feedings quiet and low-key, avoiding too much eye contact or play. This helps condition your baby to understand that nighttime is for sleeping, not socializing. Over time, as your baby grows and can go longer between feedings, these nightly sessions will become less frequent. Until then, embracing them as opportunities for closeness and nourishment can make them feel more manageable.
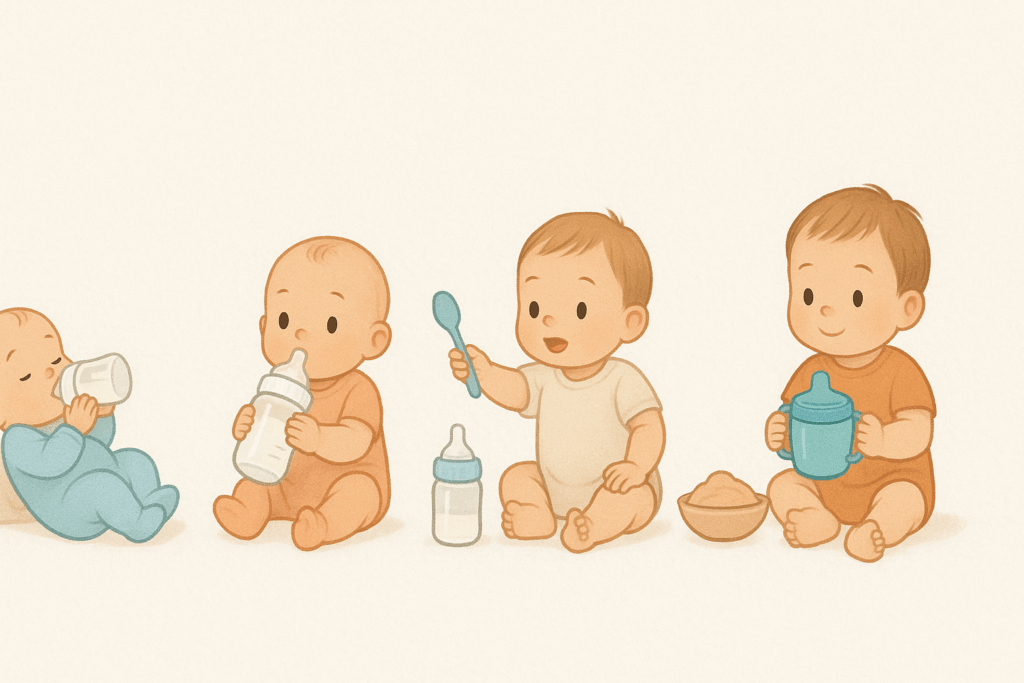
Evolving Nutritional Needs: When to Adjust Bottle Feeding as Baby Grows
As your baby progresses through the first year, their nutritional needs evolve. What worked for a newborn will likely need adjustment by the time they reach three, six, or nine months. Recognizing and responding to these changes is vital to sustaining healthy development and preparing your baby for more independent feeding habits.
In the early months, babies typically consume about 2 to 4 ounces per feeding, gradually increasing to 6 to 8 ounces by six months of age. Feeding frequency will decline as volume increases, with many infants transitioning to five or six feedings a day by the half-year mark. Alongside these changes, some babies may begin to sleep longer stretches at night, reducing the need for overnight feeds.
Introducing solid foods around six months marks another turning point. While breast milk or formula remains the primary source of nutrition until age one, solids offer additional nutrients and new textures. Bottle feeding routines should be adjusted to accommodate this shift—typically by offering solids after a bottle feed to ensure continued milk intake. Parents should be careful not to rush this transition. Babies should continue to receive a consistent supply of milk or formula to meet their foundational needs.
Watching your baby’s cues and growth markers—such as steady weight gain, developmental milestones, and satisfaction after meals—helps guide these adjustments. Pediatricians can also provide individualized guidance on how much and how often to feed as your infant grows.
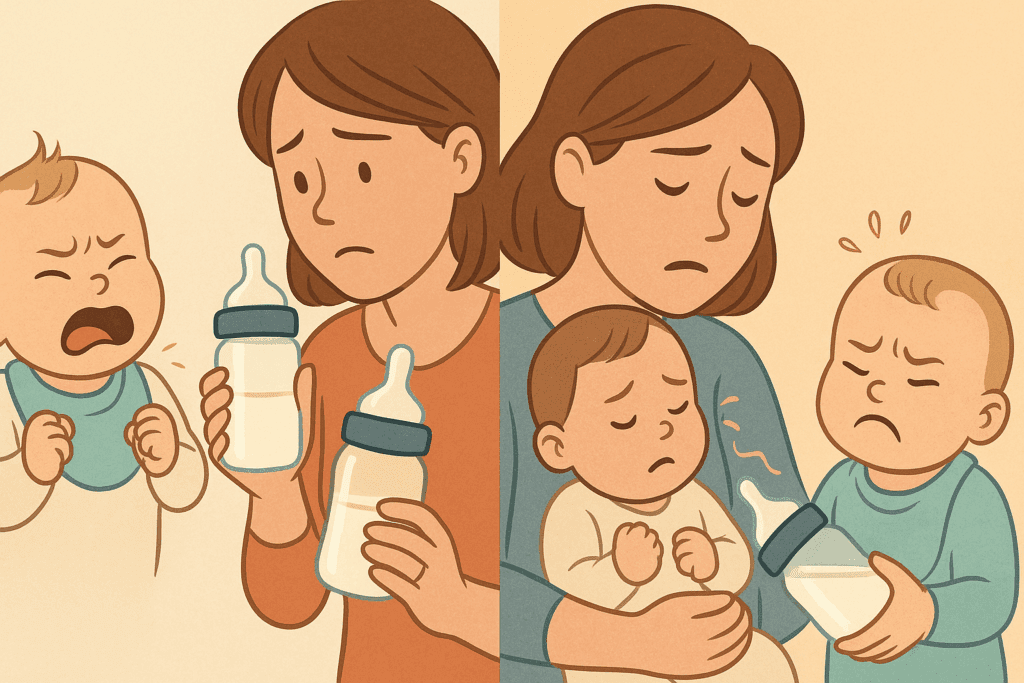
Overcoming Common Challenges in Infant Bottle Feeding
Despite preparation and effort, challenges with infant bottle feeding can arise, especially during the first few months. Some babies may reject the bottle entirely, others may suffer from colic or reflux, and some may display feeding aversions. Understanding the possible causes behind these challenges and how to respond calmly can reduce parental stress and support better feeding outcomes.
Bottle refusal is a common issue, particularly in breastfed babies transitioning to bottles. This may be due to nipple confusion, temperature preferences, or the pace of feeding. Trying different bottle nipple shapes, warming the milk to body temperature, or offering the bottle when the baby is calm and only slightly hungry may increase acceptance. Having someone other than the breastfeeding parent offer the bottle can also help, as the baby won’t be expecting the breast.
Colic, defined as excessive crying without an obvious cause, is another frequent concern. While its exact origins are unclear, it often peaks around six weeks and resolves by three to four months. Bottle feeding adjustments—such as switching to anti-colic bottles, trying hypoallergenic formula, or feeding in an upright position—can sometimes alleviate symptoms. Similarly, reflux may present as frequent spitting up, arching during feeds, or poor weight gain. In such cases, feeding more slowly, keeping your baby upright after meals, and offering smaller, more frequent feeds may help.
For persistent issues or signs of feeding distress—such as choking, gagging, coughing, or lack of weight gain—medical evaluation is essential. Sometimes, underlying conditions such as tongue-tie, allergies, or gastrointestinal sensitivities require professional intervention.
How to Bottle Feed a Newborn While Encouraging Long-Term Healthy Habits
Bottle feeding a newborn is about more than meeting immediate nutritional needs; it also shapes future attitudes toward eating, self-regulation, and trust. Responsive feeding practices—recognizing hunger and fullness cues, avoiding pressure or distraction, and creating a nurturing feeding environment—foster lifelong healthy relationships with food.
As babies grow older, they begin to understand feeding routines and expectations. Using bottle feeding time to cultivate positive rituals—such as quiet cuddling, eye contact, and gentle conversation—encourages children to view eating as a comforting, shared activity. Avoiding screens and distractions during feeding also teaches babies to focus on their internal hunger cues and recognize satiety naturally.
Over time, caregivers can gradually transition from bottle to cup, especially after the one-year mark. This helps support oral development and reduces the risk of dental issues associated with prolonged bottle use. The process should be gentle and guided by your baby’s readiness. Introduce sippy cups or open cups during meals and offer them alongside familiar bottle feeds. A smooth transition is often more successful when emotional support and routine remain consistent.
By approaching bottle feeding as a holistic practice—encompassing nutrition, bonding, behavior, and development—caregivers lay the groundwork for lifelong wellness. These early experiences shape a child’s view of food and eating for years to come.
How to Bottle Feed a Newborn in Special Situations: Prematurity, Illness, and NICU Transitions
For some families, the path to bottle feeding is complicated by special circumstances such as premature birth, medical conditions, or time spent in the neonatal intensive care unit (NICU). Learning how to bottle feed a newborn in these contexts requires flexibility, patience, and often, professional support.
Premature infants often lack the muscle tone or coordination needed for sucking, swallowing, and breathing simultaneously. Feeding may begin with a nasogastric (NG) tube and gradually transition to bottle feeding as the baby gains strength and maturity. Specialized nipples with slower flow rates, as well as paced feeding techniques, can help these infants build endurance and confidence. Occupational or speech therapists in the NICU are often involved in this transition, guiding families in safe, effective techniques tailored to each baby’s developmental stage.
In cases where a baby has a medical condition such as cleft palate, Down syndrome, or neurological impairment, feeding adaptations may be necessary. Modified bottles, positioning supports, or thickened formula may be recommended to ensure safe swallowing and adequate nutrition. Feeding specialists work closely with pediatricians to craft individualized plans and educate caregivers on best practices.
For babies who begin life in the NICU, transitioning to home feeding requires a structured but adaptable approach. Caregivers often need to learn how to track intake meticulously, administer medications if needed, and identify signs of distress or regression. Ongoing communication with a pediatric team, and sometimes early intervention services, ensures that these infants continue to thrive once they leave the hospital.
Understanding Nutritional Milestones in Bottle-Fed Infants
Nutrition is more than just caloric intake—it’s a developmental journey marked by distinct milestones that guide your baby toward more independent eating. For bottle-fed infants, these milestones include increasing volume per feed, longer stretches between feeds, the ability to self-regulate intake, and the eventual transition to solids and cups.
By three to four months, many babies begin to show signs of stronger neck control and greater interest in surroundings during feeds. Around this time, they may begin holding their bottle with assistance or demonstrating curiosity about adult food. These are natural signs of cognitive and motor development and can be encouraged by allowing your baby to participate actively in the feeding process.
Around six months, the introduction of solids is a key milestone. Bottle feeds continue to form the nutritional foundation, but exposure to purees, cereals, and soft textures allows babies to develop oral motor skills and taste preferences. Parents should continue to offer formula or breast milk first, then solids, to ensure that primary nutrition remains intact.
By nine to twelve months, many infants begin to show readiness for weaning from the bottle. They may prefer holding a sippy cup, imitating family meals, or consuming larger portions of solid food. This transition is gradual and should be guided by your baby’s readiness rather than a rigid timeline. Maintaining a supportive, relaxed feeding environment during these changes reinforces healthy habits and nurtures confidence.
Frequently Asked Questions: Expert Insights on Infant Bottle Feeding
How to Bottle Feed a Newborn When Traveling or On the Go
Traveling with a newborn presents unique challenges, especially when it comes to feeding. For families learning how to bottle feed a newborn outside the comfort of home, preparation becomes critical. Pre-measuring formula portions in airtight containers and using insulated bottle carriers can simplify the process significantly. Consider carrying pre-sterilized disposable bottles and single-use nipples if access to clean water is limited. If using expressed breast milk, a portable cooler with ice packs ensures proper storage for up to 24 hours. Whether on a plane, in a car, or at a hotel, flexibility is essential—look for feeding-friendly environments, maintain your baby’s feeding cues, and aim to recreate the calm, semi-upright position used at home. With a bit of planning, feeding while traveling can become a seamless part of your family routine.
Can Infant Bottle Feeding Affect Oral Development?
While infant bottle feeding is an effective and nourishing method, it’s important to consider its long-term effects on oral and facial development. Prolonged bottle use—especially beyond the age of 18 months—can increase the risk of dental issues, such as tooth decay and misaligned teeth. To mitigate this, caregivers should avoid putting babies to bed with a bottle and begin transitioning to a cup around their first birthday. Additionally, using orthodontic or nipple-shaped bottles can encourage natural sucking motions that support oral muscle coordination. Consulting with a pediatric dentist by the time your baby turns one can help identify early concerns and provide guidance tailored to your child’s growth trajectory.
What Role Does Pacing Play in Infant Bottle Feeding?
Paced bottle feeding is a technique that mirrors breastfeeding dynamics and helps prevent overfeeding. This method involves holding the bottle horizontally, allowing the baby to draw milk at their own pace rather than relying on gravity-driven flow. When caregivers understand how to bottle feed a newborn using paced techniques, they foster better appetite regulation and reduce the risk of choking or gulping. It also encourages the baby to pause and rest during feeding, just as they would when breastfeeding. This approach not only supports satiety recognition but can also lessen the likelihood of colic and gas. Introducing paced feeding from the outset can have a positive impact on a child’s self-regulation as they grow.
How to Bottle Feed a Newborn with a Sensitive Stomach
Feeding a baby with digestive sensitivity demands both patience and strategic adjustments. Some newborns experience discomfort due to lactose intolerance, protein sensitivity, or immature digestive systems. When learning how to bottle feed a newborn with a sensitive stomach, consider using formulas labeled as hydrolyzed or hypoallergenic under a pediatrician’s guidance. Burping more frequently—every one to two ounces—can reduce trapped air and associated discomfort. Feeding in an upright position and keeping the baby elevated for 20 to 30 minutes post-feed may also ease symptoms. If discomfort persists despite these changes, a pediatric gastroenterologist may be able to determine if there’s an underlying condition requiring specialized care.
What Are the Best Practices for Cleaning Bottles and Nipples?
Thorough cleaning and sterilization practices are essential to ensure safety in infant bottle feeding. Before first use, all feeding components should be sterilized using boiling water, a steam sterilizer, or a dishwasher with a sanitize cycle. After every feed, rinse items with cold water to remove milk residue, then wash with hot soapy water using dedicated bottle brushes. Let all parts air dry on a clean surface—avoid towel drying, which can introduce bacteria. For infants under three months or with compromised immunity, daily sterilization is strongly recommended. These hygiene practices are especially crucial when you’re just learning how to bottle feed a newborn, as their immune systems are still developing and highly vulnerable to contaminants.
Can Different Bottle Materials Affect Feeding Safety?
The material of baby bottles—typically plastic, glass, silicone, or stainless steel—can influence both safety and comfort during infant bottle feeding. Glass bottles are free of chemicals like BPA and are easy to sterilize but heavier and more prone to breakage. Plastic bottles are lightweight and durable but should always be BPA-free and replaced regularly due to wear and tear. Silicone offers flexibility and is often used for collapsible travel bottles, while stainless steel is a newer option praised for temperature retention and longevity. When choosing how to bottle feed a newborn, selecting the right material involves balancing safety, durability, and ease of use. Each family may find different materials work better depending on lifestyle and personal preferences.
How to Bottle Feed a Newborn During Growth Spurts
Growth spurts can disrupt predictable feeding routines, often leading to fussiness, frequent feedings, and changes in sleep. During these phases—commonly seen around two weeks, six weeks, three months, and six months—it’s vital to remain responsive to your baby’s evolving hunger signals. Infant bottle feeding during a growth spurt may require increasing the volume of formula or breast milk temporarily. Offering slightly more per feed or feeding more often supports the baby’s elevated metabolic needs without overloading their system. It’s also important to maintain consistent sleep cues and soothing routines to help your baby navigate these developmental leaps. Trusting your baby’s signals and adjusting feeding plans gradually are key to supporting their healthy adaptation.
Are There Long-Term Health Outcomes Linked to Bottle Feeding?
Emerging research suggests that infant bottle feeding may be associated with subtle long-term health patterns, depending on technique and feeding environment. For example, rigid feeding schedules or encouraging babies to finish bottles regardless of cues may disrupt hunger recognition and contribute to overfeeding. Conversely, responsive bottle feeding—acknowledging hunger and fullness cues—can support healthy weight trajectories and metabolic regulation. In terms of emotional development, caregivers who engage with their baby during feeds using eye contact, touch, and verbal interaction can foster strong emotional bonds, regardless of feeding method. While more studies are needed, early feeding practices are increasingly recognized as shaping not just immediate nutrition but also long-term relationships with food and emotional health.
How to Bottle Feed a Newborn Using Donor Milk Safely
When breast milk from the baby’s biological mother is unavailable or insufficient, screened donor milk is a medically endorsed alternative. For parents learning how to bottle feed a newborn with donor milk, it’s important to source milk from certified milk banks that follow FDA and HMBANA safety protocols. Donor milk is pasteurized to eliminate pathogens while preserving many beneficial nutrients and immune properties. Once received, the milk must be stored properly in a refrigerator or freezer and used within the recommended timeframe after thawing. Warming the milk gently to body temperature and handling it with the same hygiene standards as formula ensures safe feeding. Donor milk offers a valuable option for infants with special health needs or for families seeking supplemental feeding with human milk.
What Innovations Are Emerging in Infant Bottle Feeding Technology?
As baby care technology evolves, innovations in infant bottle feeding continue to emerge, offering both convenience and personalization. Smart bottles now track intake, feeding frequency, and angle to provide feedback through mobile apps, helping parents monitor patterns more accurately. Self-warming bottles are becoming increasingly popular, allowing for on-the-go feeding without the need for external warmers or microwaves. Some advanced designs include air-venting systems to reduce colic or built-in temperature indicators to ensure milk is at a safe and soothing temperature. These tools can enhance the feeding experience, especially for caregivers balancing work, travel, and infant care. As parents explore how to bottle feed a newborn using new tools, these innovations can offer peace of mind, especially when consistency and efficiency matter most.
Conclusion: Final Thoughts: Nurturing Growth Through Expert Infant Bottle Feeding
Learning how to bottle feed a newborn is more than just a mechanical skill—it’s an act of nurturing that weaves together science, intuition, and emotional presence. From those early, sleepy feedings to the more alert and engaged sessions of an older infant, each bottle becomes a moment of connection, nourishment, and growth. Whether a parent chooses to use formula, expressed breast milk, or a combination of both, what matters most is how they respond to their baby’s unique needs with consistency, love, and attentiveness.
The practice of infant bottle feeding plays a critical role in shaping early developmental trajectories. When done thoughtfully, it supports cognitive, physical, and emotional health, while building the foundation for healthy eating behaviors that will serve a child throughout their life. By mastering proper technique, understanding evolving nutritional needs, and responding to feeding challenges with knowledge and care, caregivers can confidently support their child’s journey through infancy.
As feeding patterns shift, milestones are met, and your newborn grows into a thriving, curious child, remember that the bottle is not just a tool—it’s a bridge. A bridge to independence, a bond between parent and child, and a beginning of a lifelong relationship with food, family, and health. In honoring this journey with intention and care, parents are not just feeding their babies—they are shaping futures, one bottle at a time.



