Introduction
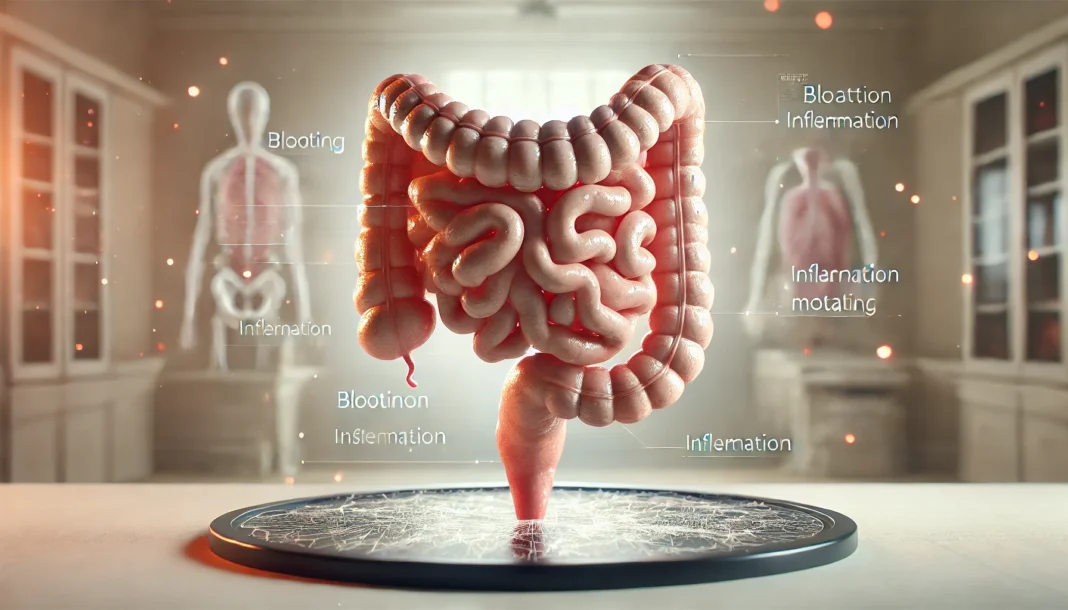
Bowel problems affect millions of people across the globe, often interfering with daily life, comfort, and health. Whether these concerns arise as occasional digestive upsets or persist as chronic conditions, understanding the underlying causes and solutions is essential for maintaining long-term gastrointestinal wellness. Bowel issues can take many forms, including irregular bowel movements, chronic constipation or diarrhea, bloating, abdominal discomfort, and visible changes in stool. These symptoms, when persistent, may be signs of more complex bowel disorders or colon issues that require medical attention and targeted care.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
Poop problems are more than just an inconvenience—they can signal imbalances or dysfunctions in the digestive tract that need to be addressed at the root level. The stigma surrounding bowel difficulties often causes individuals to delay seeking treatment, exacerbating symptoms and diminishing quality of life. However, with advancing research and greater awareness, effective diagnosis and treatment of bowel disorders are becoming more accessible. From inflammatory bowel disease to irritable bowel syndrome, structural abnormalities, and functional digestive disorders, bowel issues encompass a wide range of medical conditions that require individualized approaches.
In this comprehensive article, we explore the different types of bowel disorders, what causes them, the symptoms to recognize early, and the most effective treatments. We highlight the connection between bowel function and lifestyle factors, including diet, hydration, stress, sleep, and gut microbiota. Whether you are navigating chronic bowel difficulties or seeking preventative guidance, this article offers science-backed insights rooted in EEAT principles—Experience, Expertise, Authoritativeness, and Trustworthiness—to help you reclaim your digestive health with confidence.

Common Types of Bowel Disorders
Bowel disorders are medical conditions that impair normal bowel function and are generally classified based on their origin—functional, inflammatory, or structural. These disorders often present with overlapping symptoms, making accurate diagnosis essential for effective management. Some of the most prevalent bowel problems include:
Irritable Bowel Syndrome (IBS) is a functional disorder characterized by abdominal pain and changes in bowel habits without structural damage. People with IBS may experience chronic constipation, diarrhea, or alternating patterns, often influenced by stress, diet, and hormonal fluctuations. IBS is one of the leading causes of bowel difficulties worldwide and significantly affects quality of life.
Inflammatory Bowel Disease (IBD) includes Crohn’s disease and ulcerative colitis. These autoimmune conditions involve chronic inflammation of the gastrointestinal tract. Symptoms include bloody stools, persistent diarrhea, abdominal cramping, fatigue, and weight loss. Unlike IBS, IBD causes visible damage to intestinal tissues and often requires more intensive treatment.
Chronic Constipation involves infrequent or hard-to-pass stools, excessive straining, or a feeling of incomplete evacuation. It may be caused by poor diet, sedentary lifestyle, medication side effects, or underlying medical conditions like hypothyroidism or pelvic floor dysfunction. Constipation is a common form of bowel issue, especially in older adults and women.
Chronic Diarrhea refers to loose, watery stools occurring more than three times a day for at least four weeks. It may be caused by infections, malabsorption syndromes, medication, or chronic diseases like celiac disease. Persistent diarrhea can lead to dehydration and nutrient deficiencies if untreated.
Colon issues such as diverticulitis, colorectal polyps, or colorectal cancer also present with bowel-related symptoms. These conditions are typically detected through colonoscopy or imaging and often require medical intervention, ranging from antibiotics to surgery, depending on severity and progression.

Causes of Bowel Problems: Understanding the Underlying Triggers
The causes of bowel problems vary widely depending on the specific disorder but generally fall into several broad categories. Understanding these underlying triggers helps guide treatment decisions and improves the chances of symptom relief and long-term resolution.
Dietary factors play a major role in bowel health. Diets low in fiber and high in processed foods, saturated fats, or sugars often lead to constipation, bloating, and irregular stools. Food intolerances, such as lactose or gluten sensitivity, can also result in poop problems, gas, and discomfort. The composition of the gut microbiota is heavily influenced by diet and affects digestion, inflammation, and immunity.
Psychological stress is another significant contributor. The gut-brain axis—a bidirectional communication system between the digestive tract and the central nervous system—means that emotional and mental health can directly impact bowel function. Anxiety and depression are commonly associated with bowel disorders such as IBS, where heightened sensitivity and altered motility lead to distressing symptoms.
Genetic predisposition and family history can increase the risk of certain bowel disorders, especially IBD and colorectal cancer. Genetic mutations may influence immune responses, inflammatory pathways, and how the body interacts with gut microbes.
Infections caused by bacteria, viruses, or parasites can trigger acute bowel issues such as diarrhea or even lead to post-infectious IBS, where symptoms persist long after the infection resolves. Certain antibiotics may disrupt gut flora, causing secondary bowel difficulties.
Medications including opioids, antacids, iron supplements, and chemotherapy drugs often cause bowel dysfunction. Side effects like constipation or diarrhea should be addressed in conjunction with medication changes or supportive therapies.
Autoimmune and systemic conditions such as lupus, diabetes, or hypothyroidism can affect nerve and muscle function in the colon, contributing to bowel issues. In some cases, neurological conditions like Parkinson’s disease also impair gut motility and stool regulation.
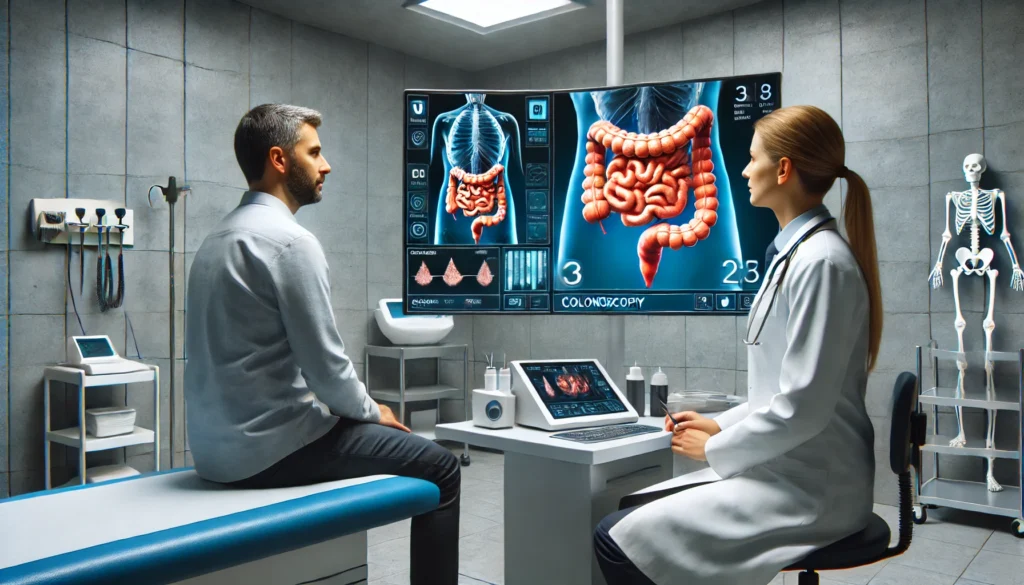
Diagnosing Bowel Disorders: What Tests and Evaluations Reveal
Accurate diagnosis is the cornerstone of effective treatment for bowel disorders. Medical evaluation typically begins with a comprehensive symptom history, dietary and medication review, and physical examination. Depending on findings, further testing may be recommended.
Colonoscopy remains one of the most important tools for detecting colon issues, allowing direct visualization of the intestinal lining and removal or biopsy of suspicious growths such as polyps or tumors. It is the gold standard for diagnosing colorectal cancer and assessing chronic inflammation in IBD.
Stool tests can identify infections, blood, fat content, or inflammatory markers such as fecal calprotectin. These tests are useful for distinguishing between inflammatory and functional causes of bowel difficulties.
Blood tests including complete blood count (CBC), C-reactive protein (CRP), thyroid panels, and electrolyte levels help detect anemia, inflammation, or systemic imbalances that may contribute to bowel problems.
Imaging studies such as CT scans, MRI, or abdominal ultrasound may be used to evaluate structural abnormalities, obstructions, or signs of inflammation not easily seen during endoscopy.
Functional tests including anorectal manometry, balloon expulsion test, or wireless motility capsules assess nerve and muscle coordination in cases of chronic constipation or suspected pelvic floor dysfunction.
Rome IV criteria are clinical guidelines used primarily to diagnose functional gastrointestinal disorders like IBS. They rely on symptom patterns and duration rather than visible pathology.

Treatment Approaches: Managing Bowel Issues Effectively
Treatment of bowel problems depends on their type, severity, and underlying causes. A combination of dietary, pharmacological, psychological, and sometimes surgical interventions is often required to provide relief and promote long-term digestive health.
Dietary modification is foundational. High-fiber diets, increased water intake, and reduction of trigger foods such as dairy, caffeine, or fermentable carbohydrates (FODMAPs) often yield significant symptom improvement. Elimination diets under medical supervision can help identify specific food intolerances that contribute to poop problems.
Pharmacologic therapy includes:
- Antispasmodics for cramping and abdominal pain
- Laxatives or stool softeners for constipation
- Anti-diarrheal agents like loperamide for loose stools
- Anti-inflammatory drugs, immunosuppressants, or biologics for IBD
- Probiotics to support healthy gut flora and immune balance
- Antibiotics for bacterial overgrowth or infections
Behavioral therapies such as cognitive-behavioral therapy (CBT), gut-directed hypnotherapy, or biofeedback address the psychological dimensions of bowel disorders. These treatments are particularly effective in IBS, reducing stress-induced symptom flares.
Surgical options may be necessary in advanced cases of colon issues, such as severe IBD with strictures, bowel obstruction, or colorectal cancer. Procedures include partial or total colectomy, resection of affected areas, or removal of polyps.
Supportive care—nutrition counseling, physical therapy, hydration management, and education—enhances long-term outcomes and helps patients regain autonomy in managing bowel difficulties.
Frequently Asked Questions
1. What are the most common signs of bowel problems?
Common signs include chronic constipation, diarrhea, bloating, abdominal cramping, mucus in the stool, urgency, and changes in stool color or consistency. These symptoms may indicate a range of bowel disorders, from functional issues like IBS to more serious colon problems such as inflammatory bowel disease or cancer. Persistent symptoms lasting more than a few weeks warrant medical evaluation.
2. How can stress impact bowel function?
Stress can significantly influence bowel issues through the gut-brain axis. Emotional distress alters gut motility, increases intestinal sensitivity, and affects the composition of gut bacteria. This connection explains why stress often worsens symptoms of IBS and other functional bowel difficulties. Mind-body therapies can improve both mental and digestive health.
3. What is the difference between IBS and IBD?
IBS (Irritable Bowel Syndrome) is a functional disorder without visible inflammation or damage, characterized by abdominal pain, bloating, and altered bowel habits. IBD (Inflammatory Bowel Disease), including Crohn’s disease and ulcerative colitis, involves chronic inflammation and can cause ulceration, bleeding, and systemic symptoms. IBD requires more intensive treatment and carries a risk of complications like strictures and cancer.
4. Are bowel issues more common in women?
Yes, bowel problems like IBS and chronic constipation are more prevalent in women. Hormonal changes during menstruation, pregnancy, and menopause influence bowel motility. Women also tend to have heightened visceral sensitivity and may experience greater stress-related symptom flares.
5. Can poop problems signal something serious?
Yes, chronic or severe poop problems may signal serious conditions such as colorectal cancer, diverticulitis, or inflammatory bowel disease. Symptoms like unexplained weight loss, blood in the stool, severe pain, or persistent diarrhea or constipation should never be ignored and require immediate medical evaluation.
6. What role does the gut microbiome play in bowel health?
The gut microbiome consists of trillions of microorganisms that aid digestion, regulate immunity, and protect against pathogens. Dysbiosis—or microbial imbalance—has been linked to bowel disorders including IBS, IBD, and even mood disorders. Probiotics and prebiotic-rich diets help support microbiome diversity and function.
7. How can I prevent chronic bowel difficulties?
Prevention strategies include maintaining a high-fiber, plant-based diet, staying hydrated, exercising regularly, managing stress, and avoiding unnecessary antibiotics. Routine screening, especially for those over 45 or with a family history of colon issues, can detect early problems before they escalate.
8. What tests are used to diagnose poop problems?
Tests include stool analysis, blood tests, colonoscopy, imaging studies, and functional assessments like manometry. These evaluations help differentiate between functional and structural causes of bowel issues and guide appropriate treatment.
9. Is there a cure for bowel disorders like IBS?
While there is no universal cure for IBS, many patients achieve long-term symptom control through lifestyle changes, diet, stress management, and medications. The key lies in understanding personal triggers and adopting a tailored, holistic approach to care.
10. When should I see a doctor about bowel problems?
You should consult a doctor if you experience symptoms such as blood in the stool, unintentional weight loss, severe or prolonged diarrhea or constipation, persistent pain, or any bowel changes lasting more than a few weeks. Early diagnosis improves treatment outcomes and reduces the risk of complications.

Conclusion
Bowel problems are a common yet often misunderstood area of digestive health. From minor poop problems to serious colon issues, these conditions impact millions and reflect a spectrum of physical, emotional, and dietary influences. Bowel difficulties not only disrupt comfort and daily life but can also indicate underlying bowel disorders that require prompt and informed care. Fortunately, with the right diagnostic tools and a personalized treatment plan, many bowel issues can be effectively managed or even prevented.
Understanding the signs and causes of bowel disorders empowers individuals to take proactive steps. From improving diet and hydration to managing stress and undergoing regular screenings, there are numerous ways to protect and support your digestive system. As science advances, so too does our ability to intervene early and improve outcomes for those suffering from chronic or acute bowel difficulties.
If you or someone you care about is facing ongoing poop problems or uncertain colon issues, don’t wait. Speak with a healthcare provider, seek expert guidance, and begin the journey to digestive resilience. The path to better bowel health is rooted in awareness, action, and support—because your gut deserves nothing less.