Introduction
Digestive discomfort can disrupt everything from your mood and energy to your focus and immunity. For many, it starts subtly—occasional bloating after meals, gas, or constipation—and slowly builds into something far more disruptive. Defects in the gastrointestinal (GI) tract can range from mild irritations to chronic illnesses that significantly impair nutrient absorption, immune response, and daily comfort. But with advancements in nutritional science and integrative medicine, it’s now possible to understand how these conditions originate—and more importantly, how to prevent them or reverse their impact. The critical questions become: can defects in the GI tract be prevented, and if not, how to fix digestive issues when they arise?
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
This article provides a comprehensive exploration of gastrointestinal health through the lens of modern science. From understanding gut anatomy and diagnosing GI tract damage to implementing personalized treatments and lifestyle interventions, this guide follows EEAT (Experience, Expertise, Authoritativeness, Trustworthiness) principles to equip readers with evidence-based answers. Whether you’re suffering from chronic indigestion or seeking long-term gut resilience, knowing how to fix digestive problems and prevent damage in the first place is essential to reclaiming wellness and vitality.
Understanding the GI Tract and Its Critical Functions
The gastrointestinal tract begins at the mouth and ends at the anus, with key organs like the esophagus, stomach, small intestine, large intestine (colon), liver, gallbladder, and pancreas orchestrating a synchronized system of digestion, absorption, detoxification, and waste elimination. Any defects in this system—whether structural, microbial, or functional—can derail not just digestion but also immune performance, neurological signaling, and inflammatory balance.
The stomach initiates the breakdown of proteins and food particles with hydrochloric acid and enzymes. The small intestine absorbs nutrients like amino acids, vitamins, and minerals. Meanwhile, the large intestine plays host to the microbiota, producing short-chain fatty acids, synthesizing vitamin K, and fermenting fiber. When any part of this chain is inflamed, obstructed, infected, or dysregulated, defects arise that manifest as digestive distress. This raises the urgent question—can defects in the GI tract be prevented with modern science? The answer is increasingly yes, especially when caught early and addressed comprehensively.

Common GI Defects: From Functional Disturbances to Structural Damage
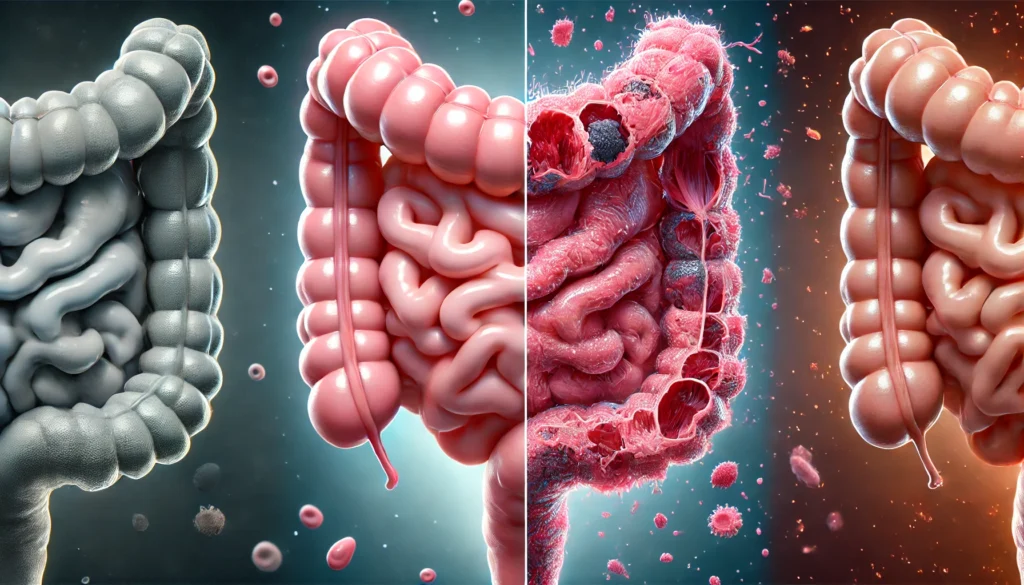
GI tract defects can range from temporary motility disturbances to chronic and irreversible damage. Functional conditions include irritable bowel syndrome (IBS), functional dyspepsia, or constipation without anatomical abnormality. Structural defects, however, may involve ulcers, strictures, diverticulosis, hiatal hernias, or even cancers that result from prolonged inflammation or unchecked microbial imbalance.
Dysbiosis—the imbalance of gut microbiota—is one of the most overlooked contributors to GI defects. A disrupted microbiome can impair epithelial barrier function, promote systemic inflammation, and reduce nutrient synthesis. Likewise, autoimmune conditions such as Crohn’s disease and celiac disease cause destructive inflammation that degrades intestinal walls. Overuse of medications like NSAIDs, excessive alcohol consumption, and dietary triggers further accelerate mucosal injury. In many cases, early intervention reveals that even seemingly inevitable damage can be reversed or prevented by modifying these environmental contributors. Knowing how to fix digestive issues at this early stage offers the best defense against long-term harm.
Risk Factors That Contribute to GI Tract Defects
The question “can defects in the GI tract be prevented?” must begin with an examination of risk factors. Lifestyle, diet, medication use, genetics, and stress all play a role. One of the most underappreciated contributors is chronic stress. Through the gut-brain axis, stress hormones like cortisol can alter motility, weaken the mucosal lining, and disturb microbial populations, all of which create fertile ground for digestive disease.
Highly processed diets low in fiber and rich in sugar, trans fats, and food additives can damage the intestinal lining, promote dysbiosis, and induce leaky gut syndrome. Meanwhile, frequent antibiotic use, acid-suppressing medications like PPIs, and lack of physical activity reduce microbial diversity and impair natural digestive processes. Age and hormonal fluctuations—especially in women—also alter GI function, making certain groups more vulnerable.
Recognizing and reducing these risk factors is one of the most practical ways to learn how to fix digestive problems before they escalate. Prevention and early response remain the twin pillars of gut resilience.
The Science of Leaky Gut and Intestinal Permeability
Leaky gut, or increased intestinal permeability, occurs when tight junctions in the epithelial lining of the gut wall become loose, allowing bacteria, toxins, and undigested food particles to escape into the bloodstream. This triggers systemic inflammation and can lead to autoimmune activation, skin disorders, allergies, and neurological symptoms. Research now links leaky gut to numerous chronic illnesses, including type 1 diabetes, rheumatoid arthritis, and multiple sclerosis.
Zonulin, a protein modulated by gluten and bacterial triggers, is one of the key regulators of intestinal permeability. Elevated levels are found in individuals with celiac disease, type 1 diabetes, and IBS. Addressing leaky gut involves removing inflammatory foods, managing stress, optimizing sleep, and using supplements such as L-glutamine, zinc carnosine, and polyphenols. If you’re asking how to fix digestive issues rooted in barrier dysfunction, healing leaky gut becomes a central strategy.

How to Fix Digestive Issues: Evidence-Based Nutritional Approaches
Fixing digestive problems starts with personalized nutritional correction. For many, the removal of food sensitivities—including gluten, dairy, soy, corn, and eggs—leads to rapid improvement. Elimination diets like low-FODMAP or specific carbohydrate diet (SCD) have shown effectiveness in IBS, SIBO, and IBD.
Anti-inflammatory diets rich in omega-3s, antioxidants, and polyphenols help reduce gut inflammation and support microbial diversity. Fermented foods like sauerkraut, kefir, and miso can repopulate beneficial bacteria. Prebiotics (inulin, resistant starch) serve as fuel for probiotics. Targeted use of digestive enzymes, bile salts, and stomach acid replacement (e.g., betaine HCl) enhances breakdown and absorption. Fiber diversity is key—aiming for 30+ plant types per week correlates with optimal microbiota health.
Understanding how to fix digestive problems through dietary precision is an essential foundation for any gut repair protocol. A qualified integrative or functional medicine practitioner can guide this process with lab testing and therapeutic diets.
Lifestyle Medicine and Stress Reduction for GI Health
Stress is one of the most powerful yet overlooked factors in gut dysfunction. Chronic stress activates the sympathetic nervous system, reduces vagal tone, and slows peristalsis—disrupting digestion at multiple levels. Meditation, yoga, breathwork, and biofeedback have demonstrated benefits for motility, pain perception, and microbial balance.
Sleep deprivation compromises gut barrier function and reduces microbial diversity, while sedentary behavior slows digestion and increases gas retention. Regular movement—including walking, stretching, and core engagement—enhances circulation to the gut and stimulates bowel function. Even more compelling is the bidirectional benefit: as gut health improves, mental clarity, mood, and emotional regulation also stabilize.
A comprehensive strategy that includes nervous system support is central to learning how to fix digestive problems holistically. Gut repair isn’t just about food—it’s about restoring balance across all body systems.
Advanced Diagnostics: How to Identify Root Causes
Many people try multiple supplements or diets without knowing the root cause of their symptoms. Modern functional testing now offers a precision-based path to answer the question, “can defects in the GI tract be prevented or reversed?”
Comprehensive stool tests can identify dysbiosis, inflammation markers (e.g., calprotectin, lactoferrin), enzyme deficiencies, and microbial imbalances. SIBO breath tests measure hydrogen and methane gases indicative of bacterial overgrowth. Food sensitivity panels, intestinal permeability assays (zonulin, LPS), and organic acid testing provide additional layers of clarity.
Endoscopy and colonoscopy remain vital for structural evaluation, particularly in cases of bleeding, pain, or suspected malignancy. But for chronic digestive symptoms without clear findings, functional diagnostics often uncover the hidden culprits. Armed with this data, clinicians can create precise, personalized protocols to fix digestive problems effectively.

Probiotics, Prebiotics, and the Microbial Restoration Model
Restoring the microbiome is a cornerstone of any gut-healing protocol. Probiotics introduce beneficial organisms that compete with pathogens, improve motility, enhance immune function, and reinforce the gut lining. However, not all probiotics are created equal. Strain-specific effects matter—Lactobacillus plantarum may reduce bloating, while Bifidobacterium infantis helps with IBS pain.
Prebiotics, such as galacto-oligosaccharides and arabinogalactans, feed beneficial microbes and enhance butyrate production, a short-chain fatty acid essential for gut wall integrity. Synbiotics combine both elements for synergistic effect. Fecal microbiota transplantation (FMT), while still experimental for many conditions, has proven effective in refractory C. difficile infections and shows promise in ulcerative colitis.
When considering how to fix digestive issues, a strategic, phased approach to microbiome repair—with dietary, supplemental, and environmental modifications—is key. It’s not just about adding bacteria, but about creating the right ecosystem for them to thrive.
Pediatric and Geriatric GI Considerations
Children and the elderly have unique vulnerabilities to GI tract defects. Pediatric GI problems often stem from food allergies, immature gut development, or microbiome disruption due to C-sections and antibiotic exposure. Constipation, colic, and food sensitivities are common early indicators that digestive resilience needs support.
In older adults, gastric acid levels decline, enzyme production drops, and microbial diversity narrows. These shifts increase the risk of malabsorption, infections, and inflammatory bowel conditions. Understanding how to fix digestive problems in these populations involves tailored interventions: age-appropriate fiber, enzyme support, hydration, and careful medication management.
Aging does not have to mean digestive decline. With proactive strategies, both children and seniors can maintain healthy, functional digestive systems throughout life.
Frequently Asked Questions
1. Can defects in the GI tract be prevented with lifestyle changes?
Yes, many GI tract defects can be prevented or minimized through diet, stress reduction, sleep hygiene, and physical activity. By reducing inflammatory triggers, supporting microbial health, and improving motility, you can build resilience against both functional and structural gut damage. Early prevention remains more effective than late-stage intervention.
2. What are the first signs that digestive problems are developing?
Early signs include bloating, gas, heartburn, irregular bowel movements, food sensitivities, fatigue, and skin issues. These symptoms often precede more serious conditions like IBS, IBD, or leaky gut. Recognizing and addressing them promptly is key to avoiding long-term complications.
3. How can I tell if my digestive problems are caused by diet?
Keeping a food and symptom journal helps correlate reactions to specific foods. Elimination diets, followed by reintroduction phases, can identify triggers. Lab testing for food sensitivities or IgG antibodies adds further precision. A dramatic improvement in symptoms after dietary changes often confirms food-related origins.
4. Are probiotics enough to fix digestive issues?
Probiotics are powerful tools but not standalone solutions. Their effectiveness depends on strain, dosage, and your existing microbiome. For lasting results, they must be part of a broader strategy that includes diet, lifestyle, and stress management. Without addressing root causes, probiotics may offer only temporary relief.
5. What role does hydration play in digestive health?
Hydration supports motility, nutrient absorption, enzyme function, and mucosal barrier integrity. Dehydration can cause constipation, reduce stomach acid, and impair detoxification. Drinking filtered water throughout the day, especially with fiber intake, ensures optimal digestive function.
6. Can chronic digestive problems affect mental health?
Absolutely. The gut-brain axis links gut function with mood, cognition, and emotional resilience. Imbalances in gut bacteria can contribute to anxiety, depression, and brain fog. Conversely, addressing digestive issues often improves mental clarity, focus, and emotional regulation.
7. What tests help identify GI defects before symptoms become severe?
Stool analysis, food sensitivity testing, zonulin levels, and SIBO breath tests offer early insights into microbial, immune, and barrier dysfunction. These tests can detect imbalances long before structural damage becomes evident, allowing for earlier intervention.
8. How long does it take to fix digestive problems naturally?
Healing timelines vary but typically range from several weeks to several months. Minor imbalances may resolve in 4–6 weeks, while deeper issues like leaky gut or SIBO can take 3–6 months or longer. Consistency, personalization, and professional guidance significantly improve outcomes.
9. Are digestive enzyme supplements safe to use long-term?
When used appropriately and under medical supervision, digestive enzymes are safe and often necessary in cases of pancreatic insufficiency, gallbladder removal, or age-related decline. However, they should be paired with efforts to restore endogenous enzyme production through dietary and lifestyle changes.
10. What is the most important step in preventing GI tract defects?
The most important step is awareness—knowing your risk factors, monitoring your symptoms, and taking proactive measures. Balanced nutrition, reduced toxin exposure, and regular screening allow you to detect and prevent issues early. Education is the foundation of prevention.

Conclusion
The digestive system lies at the heart of overall health, influencing immunity, energy, mood, and longevity. Defects in the GI tract—whether functional or structural—can quietly undermine your well-being for years before more serious symptoms emerge. But science now shows us that prevention and reversal are often possible with the right tools.
By asking critical questions like “can defects in the GI tract be prevented?” and “how to fix digestive issues effectively?” you begin a path of self-empowerment. The answers lie not in temporary relief, but in a comprehensive, patient-centered approach that includes diagnostic clarity, nutritional strategy, microbial balance, and lifestyle optimization.
Whether you’re already struggling with chronic symptoms or simply want to safeguard your long-term health, this is your moment to act. The GI tract isn’t just a pipeline—it’s a biological command center that, when restored, enhances every system it touches. Prioritizing your gut is one of the most impactful health decisions you can make—and the science says it’s never too late to start.