Introduction
Living with chronic digestive discomfort, inflammation, or unexplained bowel symptoms can be a life-altering challenge that affects physical well-being, emotional health, and overall quality of life. For millions around the world, these struggles are rooted in a misunderstood yet medically complex group of disorders known as inflammatory bowel disease (IBD). From early signs of inflamed intestines to navigating the intricate web of colitis medicine, the path to diagnosis, management, and long-term healing can feel overwhelming and uncertain.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
This comprehensive article demystifies the questions patients and caregivers often have—what is IBD, how to treat it, and what to expect from the range of colitis treatments and gut inflammation protocols available today. Whether you’ve recently been diagnosed, are wondering about inflammatory bowel syndrome symptoms, or have battled flare-ups for years, understanding how to calm inflamed intestines and achieve remission is essential to living fully.
We explore the latest in ibd treatment science, the roles of different inflammatory bowel disease medications, and how to soothe inflamed intestines with both evidence-based and integrative strategies. You’ll also find insights into diagnosis, monitoring, the timeline for healing, and how to treat colon inflammation from both acute and long-term perspectives.
Ultimately, this guide brings together the most current research and trusted medical insights to empower you with clarity, confidence, and control over your inflammatory bowel condition.
What Is IBD? Understanding the Foundation of Inflammatory Bowel Disease
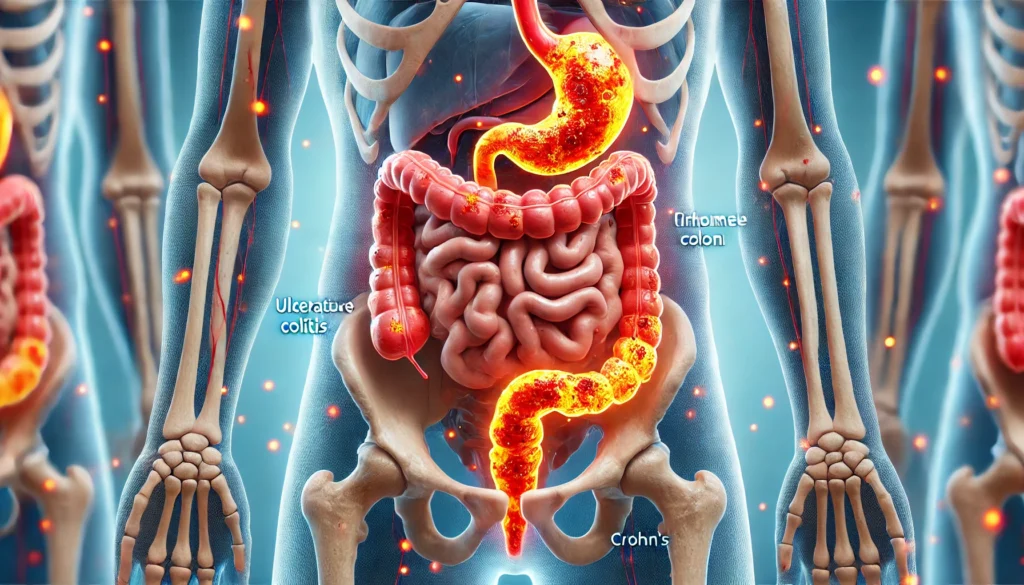
Inflammatory bowel disease (IBD) refers to a group of chronic disorders that cause prolonged inflammation of the gastrointestinal (GI) tract. The two primary types of IBD are Crohn’s disease and ulcerative colitis. While often confused with irritable bowel syndrome (IBS), IBD is different in that it results in physical damage and inflammation of the bowels, as confirmed by diagnostic tests and biopsies.
Understanding what is IBD requires acknowledging its autoimmune and inflammatory roots. In IBD, the immune system mistakenly attacks healthy tissue in the gut, leading to symptoms like persistent diarrhea, abdominal pain, fatigue, weight loss, and rectal bleeding. These conditions may fluctuate between flare-ups and remission, with symptoms that are at times debilitating.
Crohn’s disease can affect any part of the digestive tract from the mouth to the anus but most commonly impacts the terminal ileum. It is characterized by inflammation that can penetrate deep into intestinal walls. Ulcerative colitis, by contrast, typically involves only the colon and rectum and presents with continuous areas of superficial inflammation.
IBD is a lifelong condition, but modern ibd treatment approaches have transformed the management of symptoms, allowing many patients to achieve long periods of symptom control and improved quality of life.

Recognizing Inflamed Bowel Symptoms and Early Red Flags
Early detection plays a critical role in effective intervention. Recognizing inflamed bowel symptoms can help distinguish IBD from more benign gastrointestinal issues like IBS, infections, or food intolerances. Some of the most commonly reported signs of inflammation of the bowels include persistent abdominal cramping, diarrhea that lasts longer than two weeks, visible blood in stool, unintentional weight loss, fatigue, and a constant sense of urgency even without a bowel movement.
In children and adolescents, growth delays or failure to thrive may indicate small bowel inflammation. Adults may also notice joint pain, skin rashes, or eye inflammation—extraintestinal manifestations that often accompany IBD flare-ups.
Many patients confuse symptoms with common digestive disturbances, delaying the pursuit of treatment for inflamed bowel. This delay may worsen tissue damage or increase the risk of complications such as strictures, fistulas, or colorectal cancer. That’s why any prolonged or escalating GI symptom pattern warrants medical evaluation and, when indicated, an ibd diagnostic test.
Understanding these early warning signs also helps patients better monitor the progression of their illness and recognize when to escalate or adjust ibd disease treatment strategies.
IBD Diagnostic Test Methods: How Is IBD Diagnosed?
Diagnosis of IBD involves a multifaceted approach, beginning with a detailed clinical history and followed by a combination of lab tests, imaging studies, and endoscopic procedures. Because there is no single definitive test, confirming inflammatory bowel disease requires the exclusion of other conditions and the identification of tell-tale tissue changes or inflammatory markers.
Blood tests often reveal elevated inflammatory proteins such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), alongside anemia or vitamin deficiencies. Stool tests like fecal calprotectin can indicate intestinal inflammation and help differentiate IBD from IBS. These are frequently ordered as preliminary steps before more invasive testing.
Endoscopy remains a cornerstone of diagnosis. A colonoscopy allows direct visualization of the colon and terminal ileum and enables biopsies of suspicious areas. In Crohn’s disease, inflammation may appear patchy and deeper, whereas in ulcerative colitis, inflammation tends to be continuous and limited to the mucosal layer.
Advanced imaging techniques such as MRI enterography or CT enterography are used to assess the small bowel, especially in suspected cases of small bowel inflammation. Capsule endoscopy, in which a tiny camera is swallowed, may also detect lesions unreachable by standard endoscopes.
Ultimately, the diagnosis of IBD is confirmed through a combination of visual evidence, histological patterns, clinical presentation, and laboratory results. Accurate diagnosis not only informs prognosis but also guides appropriate ibd disease treatment from the outset.
Inflammation of the Bowels: Why It Happens and How It Affects the Body
Inflammation of the bowels is the body’s immune response to perceived threats within the gastrointestinal lining. In IBD, this response becomes chronic and misdirected. Environmental triggers, genetic predisposition, and dysbiosis (an imbalance in gut microbiota) all contribute to this autoimmune-like reaction.
Once inflammation begins, immune cells such as neutrophils, macrophages, and T-cells infiltrate the intestinal walls, releasing cytokines that damage tissues and perpetuate inflammation. Over time, this leads to ulceration, thickening of the intestinal wall, loss of absorptive capacity, and a disrupted mucosal barrier.
The long-term effects of untreated inflammation include strictures (narrowing of the bowel), fistulas (abnormal connections between organs), abscesses, and malnutrition. Systemic inflammation can also impact joints, liver function, and bone density.
Managing inflammation of the bowels requires understanding how to calm intestinal inflammation both acutely and preventatively. Suppressing the immune response while promoting mucosal healing is the goal of most modern ibd treatment strategies.
Colitis Medicine and IBD Treatment Options
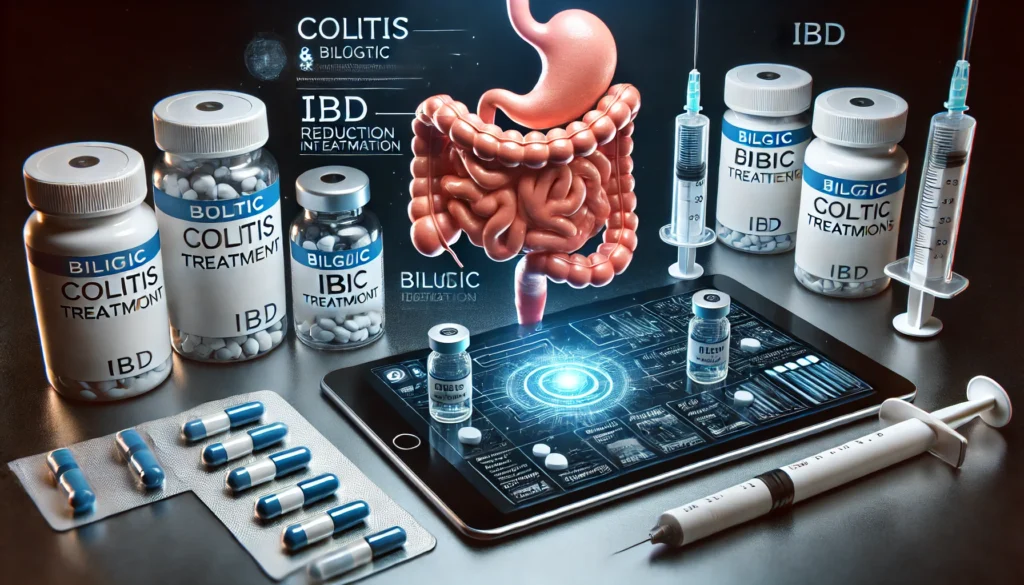
Colitis medicine and Crohn’s disease therapies have evolved considerably in recent decades. The goal of ibd treatment is to induce remission, maintain long-term symptom control, and prevent complications. Treatment plans are tailored based on the severity, location, and pattern of inflammation, as well as individual patient response.
First-line treatments for mild-to-moderate inflammation often include 5-aminosalicylic acid (5-ASA) drugs such as mesalamine. These are typically used in ulcerative colitis and work by delivering anti-inflammatory action directly to the colon lining. Though not always effective for Crohn’s, they remain a foundational class of colitis treatments.
Corticosteroids like prednisone may be used during acute flare-ups. While highly effective in reducing inflammation quickly, their long-term use is discouraged due to serious side effects, including osteoporosis, weight gain, and immune suppression.
Immunomodulators such as azathioprine, 6-mercaptopurine, and methotrexate help maintain remission by modulating the immune system. These drugs for inflammatory bowel disease are particularly useful in steroid-dependent patients or those who cannot tolerate biologics.
Biologic therapies, including anti-TNF agents (like infliximab and adalimumab), anti-integrin agents (vedolizumab), and IL-12/23 blockers (ustekinumab), represent a modern revolution in ibd disease treatment. They target specific immune pathways to stop inflammation at its source and are effective for both moderate and severe cases.
Newer small molecule drugs, such as Janus kinase (JAK) inhibitors, are expanding the landscape of inflammatory bowel disease medications, especially for patients unresponsive to biologics.
When complications arise, such as obstruction, perforation, or cancer risk, surgical interventions may be necessary. Colectomy, ileal pouch-anal anastomosis (IPAA), or bowel resection are options depending on disease location and extent.
Combining the right colitis medicine with lifestyle support and regular monitoring is critical for durable remission and improved quality of life.
How to Treat IBD with a Comprehensive, Patient-Centered Plan
Treating IBD goes far beyond prescribing medication. A holistic, patient-centered approach involves lifestyle changes, stress management, dietary adjustments, and regular medical follow-up. For those seeking how to treat ibd in a sustainable way, addressing both physiological and emotional components is key.
Dietary interventions often begin with identifying and eliminating trigger foods. While no single diet cures IBD, many patients benefit from low-residue diets during flares, or more structured protocols like the Specific Carbohydrate Diet (SCD) or low FODMAP diet under professional supervision. Nutritional deficiencies, particularly in iron, vitamin D, B12, and calcium, must be corrected to support immune function and healing.
Stress reduction is another essential element. Psychological stress has been shown to exacerbate inflammation and may trigger flare-ups. Techniques such as cognitive-behavioral therapy, mindfulness, and gut-directed hypnotherapy have demonstrated effectiveness in reducing symptoms and improving outcomes.
Regular exercise can also reduce systemic inflammation and improve overall well-being. However, exercise should be adapted to energy levels and symptom severity.
IBD support groups, both in-person and online, offer emotional support and shared coping strategies, helping reduce feelings of isolation. Collaborative care involving gastroenterologists, dietitians, mental health providers, and primary care physicians ensures a balanced and responsive treatment plan.
Ultimately, successful management depends on personalizing the ibd treatment strategy to the patient’s disease type, life stage, symptom burden, and treatment goals.
How to Calm Inflamed Bowels and Soothe the Gut Naturally
While medication plays a primary role, many patients ask how to calm inflamed bowels using complementary therapies. Natural anti-inflammatories and gut-soothing practices can provide added symptom relief and reduce reliance on aggressive medications during remission.
Certain herbal remedies such as curcumin (from turmeric), boswellia serrata, and slippery elm have shown promise in reducing gut inflammation, though they should be used under professional guidance due to variability in product quality and interactions with medications.
Probiotics, especially strains like E. coli Nissle 1917 and certain lactobacillus species, may help restore microbiota balance, particularly in ulcerative colitis. While evidence in Crohn’s is less conclusive, ongoing research continues to explore their supportive role.
Omega-3 fatty acids from fish oil or flaxseed are known to reduce systemic inflammation and may benefit IBD patients with minimal side effects.
Gentle abdominal massage, warm compresses, and stress-relieving practices like yoga or breathing exercises can help soothe gut discomfort and support parasympathetic nervous system activation, which promotes digestive healing.
Understanding how to calm inflamed intestines through both conventional and natural means can offer patients a more integrative path to wellness.

Healing Time and Expectations: How Long Does It Take for Inflamed Intestines to Heal?
One of the most pressing concerns for patients is how long does it take for inflamed intestines to heal. The answer varies widely depending on disease severity, treatment compliance, and individual immune response.
Acute flares may subside within a few weeks of proper treatment. For some, remission may begin after just a few days of corticosteroids or biologics. However, achieving deep mucosal healing—a more durable goal—often takes several months and is monitored through repeat endoscopy or biomarker testing.
Patients with longstanding, severe inflammation or complications like strictures may require years of combined medical and surgical therapy before achieving stability. Healing is not always linear, and flares can occur even during apparent remission.
Setting realistic expectations, maintaining open communication with healthcare providers, and adhering closely to prescribed regimens are essential to progress. Regular follow-ups ensure adjustments can be made swiftly if symptoms return.
Tracking symptoms, medication side effects, and triggers can also accelerate healing by identifying what works and what doesn’t. Personalized timelines, rather than one-size-fits-all predictions, are the best way to frame your healing journey.
Frequently Asked Questions
1. What is IBD and how is it different from IBS?
Inflammatory Bowel Disease (IBD) encompasses chronic conditions like Crohn’s disease and ulcerative colitis that cause actual inflammation and damage to the gastrointestinal tract. Irritable Bowel Syndrome (IBS), by contrast, involves symptoms like pain and altered bowel habits without visible inflammation or structural abnormalities. IBD requires medical treatment and ongoing monitoring, while IBS is often managed with lifestyle and dietary changes alone.
2. How do you treat colitis effectively during a flare-up?
Treating colitis during a flare involves using anti-inflammatory medications like corticosteroids or biologics to reduce active inflammation, along with dietary modifications to minimize irritation. In more severe cases, hospitalization for IV steroids, hydration, or surgical evaluation may be required. Long-term maintenance therapy follows once the flare resolves to prevent future episodes.
3. What are the early signs of inflamed intestines I should look out for?
Common early signs include persistent diarrhea, cramping abdominal pain, blood or mucus in stool, fatigue, and unexplained weight loss. Symptoms may come and go, but chronic patterns or escalation should prompt medical evaluation and possibly an ibd diagnostic test.
4. What are the most common drugs for inflammatory bowel disease?
The most commonly used medications include mesalamine, corticosteroids, immunosuppressants like azathioprine, and biologics such as infliximab or adalimumab. Newer drugs like JAK inhibitors or IL-23 blockers may also be prescribed. The choice depends on disease type, location, severity, and response to prior treatments.
5. Can diet alone treat IBD or calm inflamed bowels?
While diet alone is not a cure for IBD, it plays a crucial role in managing symptoms and supporting remission. Certain diets, such as the Specific Carbohydrate Diet or low-FODMAP diet, can reduce bloating, diarrhea, and inflammation triggers. Working with a dietitian ensures nutritional adequacy while calming inflamed bowels.
6. How is IBD diagnosed, and do I always need a colonoscopy?
IBD is diagnosed using a combination of blood tests, stool samples, imaging, and endoscopic procedures like colonoscopy. While not always immediately necessary, colonoscopy remains the gold standard for identifying mucosal damage, taking biopsies, and confirming disease extent and location.
7. What are the risks of untreated inflammation of the bowels?
If left untreated, chronic bowel inflammation can lead to complications such as strictures, abscesses, fistulas, and an increased risk of colorectal cancer. Nutritional deficiencies, growth delays in children, and systemic inflammation affecting the joints, eyes, or liver are also possible.
8. How can I calm an inflamed colon naturally?
Natural methods include reducing dietary irritants, using anti-inflammatory supplements like turmeric or omega-3s, practicing stress reduction techniques, and applying warmth to the abdomen. Probiotic use and gentle movement, such as yoga, may also help relax the colon and reduce symptom severity.
9. What’s the difference between small bowel inflammation and colon inflammation?
Small bowel inflammation often leads to malabsorption, nutrient deficiencies, and weight loss, while colon inflammation typically presents with diarrhea, urgency, and rectal bleeding. Crohn’s disease more commonly affects the small intestine, whereas ulcerative colitis is confined to the colon and rectum.
10. What should I expect from colitis disease treatment long term?
Long-term treatment involves maintenance therapy to prevent flares, monitoring for complications, and adjusting medications based on disease activity. Many patients achieve long-term remission with the right combination of colitis medicine, lifestyle changes, and medical support. Surgical options are available for those with refractory disease or complications.
Conclusion
Inflammatory bowel disease is a lifelong condition, but it is one that can be managed, understood, and treated effectively with the right strategies. Whether you are newly diagnosed or navigating persistent symptoms, knowing what is IBD, recognizing inflamed bowel symptoms early, and accessing appropriate ibd treatment is key to regaining control over your health.
Today’s therapeutic landscape—from advanced colitis medicine to precision biologics and gut-friendly dietary protocols—offers more hope than ever before. Equally important is understanding how to calm inflamed intestines through integrative care, emotional support, and lifestyle alignment. Healing begins not just with prescriptions, but with informed action, consistent follow-up, and self-compassion.
By committing to both the science of treatment and the art of daily self-care, patients can build a life beyond symptoms. The gut may be inflamed, but your ability to heal, adapt, and thrive is always intact. With every informed step, you move closer to health—not just of the body, but of the mind, community, and future.



