Introduction
Pain in the digestive tract is more than just an inconvenience—it’s a profound disruption to daily life. For many individuals, symptoms like colon pain, stomach cramps before pooping, or abdominal pain during bowel movements are not isolated occurrences. They often signal a more persistent issue, such as a spastic colon or spastic bowel, which can dramatically affect one’s quality of life. These symptoms, while common, are complex, deeply personal, and frequently misunderstood or misdiagnosed.
You may also like: The Science of Gut Repair: How to Heal Leaky Gut Syndrome Naturally with a Proven Gut Healing Diet
When patients experience abdominal cramps before bowel movement, colon spasms, or even pain in lower stomach before bowel movement, they are often left with more questions than answers. Spastic colon syndrome, a non-inflammatory functional bowel disorder, is one of the most commonly diagnosed gastrointestinal conditions, and yet it’s shrouded in confusion. The symptoms vary in severity and frequency, and they can be mistaken for other gastrointestinal issues, making accurate diagnosis and effective treatment a real challenge.
In this detailed exploration, we’ll dissect the science and symptoms behind conditions like spastic colon, irritable bowel syndrome and nausea, and bowel movement discomfort. From what causes gastrointestinal spasms to understanding why your colon hurts after pooping, this article offers an in-depth, evidence-based look at every angle. We’ll examine not only the physiological and neurological causes but also the emotional and dietary factors that contribute to these distressing symptoms.
Whether you’re navigating colon cramps, experiencing an ache in colon, or wondering about the relationship between stress and irritable bowel nausea, you’ll find clarity, support, and science-backed solutions here. This guide is designed for anyone suffering from pain in stomach while pooping or searching for answers about why their bowels hurt before and after defecation. With insights from gastroenterology, neurogastroenterology, and behavioral health, this comprehensive breakdown brings both understanding and hope to those dealing with the daily challenges of spastic colon and bowel discomfort.
The Nature of Spastic Colon: More Than Just a Digestive Problem
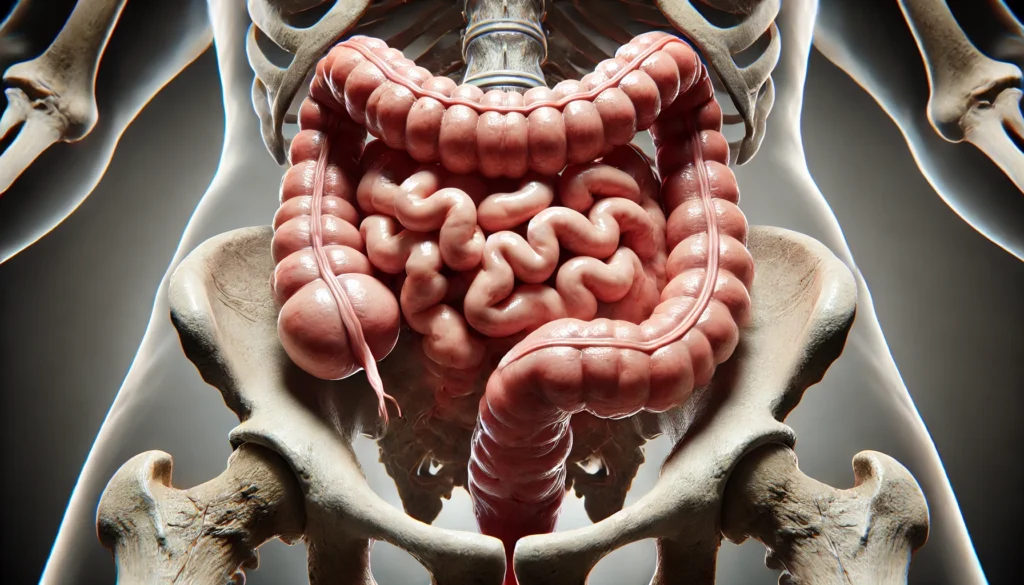
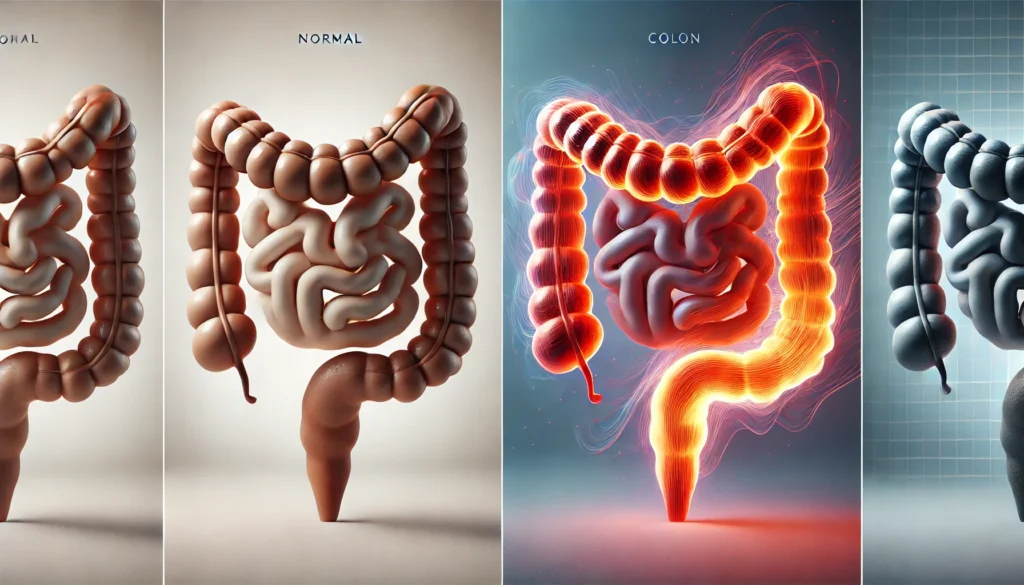
Spastic colon, also commonly referred to as irritable bowel syndrome (IBS), is a functional gastrointestinal disorder characterized by recurrent abdominal pain and altered bowel habits. Unlike inflammatory bowel diseases (IBD) like Crohn’s or ulcerative colitis, spastic colon does not involve visible inflammation or structural abnormalities in the gastrointestinal tract. Yet the symptoms can be just as severe, ranging from persistent colon cramps and stomach cramps before pooping to intense pain in lower stomach before bowel movement and unpredictable bowel habits.
At the core of this disorder lies the colon’s abnormal muscular activity. Normally, the colon contracts rhythmically to move waste material through the large intestine. In a spastic bowel, however, these contractions become irregular and overactive, resulting in colon spasms that trigger discomfort and cramping. This explains symptoms like a cramp when poop is imminent, or even sudden intestinal pain after pooping.
What differentiates spastic colon syndrome from other gastrointestinal conditions is its deeply intertwined relationship with the nervous system. The enteric nervous system—sometimes called the “second brain”—plays a crucial role in regulating gut function. In patients with a spastic colon, there may be heightened sensitivity and dysregulation of this system, leading to an overreaction to normal stimuli such as food intake or stress.
Interestingly, many patients also experience symptoms beyond the colon itself. Irritable bowel syndrome and nausea, IBS vomiting, and even systemic fatigue are frequently reported. This reinforces the theory that spastic colon is not simply a localized gut issue, but rather a full-body syndrome involving neurological, hormonal, and immune responses.
Importantly, spastic colon syndrome is not a one-size-fits-all diagnosis. Some patients primarily suffer from diarrhea, others from constipation, and many experience an alternating pattern. Regardless of the subtype, the resulting discomfort—be it bowel movement discomfort or stomach hurts during bowel movement—can significantly interfere with one’s lifestyle, mood, and overall health.
Colon Spasms and Cramping: What’s Really Happening in Your Gut?
Colon spasms are the hallmark of spastic colon and related disorders. These spasms are sudden, involuntary muscle contractions in the large intestine that may last for seconds or several minutes. For those experiencing pain in stomach while pooping or colon cramps throughout the day, these spasms are more than a medical curiosity—they are deeply disruptive events that can derail daily functioning and even social life.
The causes of colon spasm are multifactorial. One major contributor is visceral hypersensitivity, a condition in which the nerves of the gastrointestinal tract become overly responsive to even minor stimulation. This explains why some individuals experience stomach cramps before bowel movement or ache in colon even when there’s no actual obstruction or disease present.
Dietary triggers are also a major factor in spastic colon. Foods high in fat, caffeine, artificial sweeteners, or fermentable carbohydrates can exacerbate symptoms. These “FODMAPs” (fermentable oligo-, di-, monosaccharides and polyols) are poorly absorbed in the small intestine and can ferment in the colon, causing gas, bloating, and triggering colon spasms. This also sheds light on the persistent question: what causes bowel spasms? In many cases, diet is the immediate culprit, acting on an already sensitive digestive system.
Stress and anxiety also play a pivotal role in bowel spasm development. The brain-gut connection is a powerful pathway, and psychological distress can directly affect the motility and sensitivity of the colon. This is why many individuals report abdominal pain during bowel movement in times of stress, or even experience nausea, vomiting, or IBS puking in acute episodes.
Moreover, emerging research suggests a possible role of microbiome imbalance in triggering large intestine discomfort and abnormal colon activity. The gut microbiota helps regulate immune function, nerve signaling, and the integrity of the gut lining. Disruptions in this microbial ecosystem may promote inflammation and hypersensitivity, leading to recurring abdominal cramps after defecating and persistent bowel movement discomfort.

Pain Before, During, and After Bowel Movements: The Full Cycle
When patients describe stomach cramps before pooping or pain in lower stomach before bowel movement, they are often experiencing a pre-motility response where the colon begins to contract in anticipation of stool passage. These contractions, though part of a normal physiological process, become painful and exaggerated in individuals with spastic bowel.
During defecation, pain may persist or intensify. Some individuals report pain in stomach while pooping, a sign that the anal sphincter and pelvic floor muscles may also be involved. Improper coordination of these muscles—sometimes referred to as dyssynergic defecation—can make elimination painful and incomplete, causing even more distress.
Post-defecation pain, such as intestinal pain after pooping or lower abdominal discomfort after bowel movement, is another common concern. In a healthy colon, muscular activity should settle after bowel emptying. But in those with colon spasms symptoms, the colon may continue to contract or remain tense, causing lingering ache in colon or a sensation that the bowels hurt even after the movement is complete.
This cycle—cramping before, pain during, and discomfort after—can become a relentless pattern, affecting not only physical well-being but also mental health. Anticipatory anxiety before bathroom visits can exacerbate the symptoms further, leading to social withdrawal, embarrassment, and reduced quality of life.
For many individuals, these symptoms aren’t just annoying—they’re profoundly isolating. The unpredictability of flare-ups, combined with discomfort like stomach cramps while pooping or bowel spasms in public, can make daily routines daunting. Understanding and interrupting this cycle is essential for symptom relief and improved mental resilience.
Irritable Bowel Syndrome, Nausea, and Vomiting: When the Gut Feels Sick
One of the lesser-discussed aspects of spastic colon syndrome is its systemic reach. Beyond colon pain and cramps, patients often experience irritable bowel syndrome and nausea, and in more severe cases, IBS vomiting or IBS puking. These symptoms are not incidental—they are integrally connected to the disorder’s pathophysiology.
The enteric nervous system, which controls gut function, is closely connected to the central nervous system. This connection, known as the gut-brain axis, means that distress in the gut can manifest as full-body malaise, nausea, and vomiting. It’s not unusual for someone experiencing colon cramps or pain in lower stomach before bowel movement to also feel lightheaded, dizzy, or nauseated.
These symptoms also reinforce the importance of distinguishing between gastrointestinal disorders. Nausea and vomiting in the context of spastic colon are generally functional and non-inflammatory, but if left unchecked, they can lead to nutritional deficiencies, dehydration, and even psychological distress. The emotional burden of having to anticipate nausea after every meal or fear vomiting in public is immense.
Additionally, irritable bowel nausea often occurs independently of meals, further complicating its relationship with food intake. Some individuals find themselves restricting their diet in hopes of preventing nausea or cramps, leading to malnutrition and further gut imbalances.
While these symptoms may seem extreme for a non-inflammatory condition, they highlight the importance of holistic care for spastic colon syndrome. Treatments must not only target colon spasms and abdominal pain during bowel movement but also address nausea management, psychological support, and nutritional rehabilitation.

Frequently Asked Questions
1. What is a spastic colon and how is it different from inflammatory bowel disease?
A spastic colon, often used interchangeably with irritable bowel syndrome (IBS), is a functional disorder characterized by abnormal colon motility, colon pain, and sensitivity without visible inflammation or damage. In contrast, inflammatory bowel diseases like Crohn’s or ulcerative colitis involve immune-mediated inflammation, visible tissue damage, and higher risk of complications like fistulas and strictures. While both can present with abdominal cramps before bowel movement or intestinal pain after pooping, the underlying mechanisms and treatment approaches differ significantly. Spastic colon focuses more on managing symptoms through dietary, psychological, and gut-motility-based treatments. IBD typically requires immunosuppressants or biologics due to its autoimmune nature.
2. Why does my colon hurt after I poop?
Pain after defecation, including intestinal pain after pooping or ache in colon, is usually due to prolonged colon spasms or incomplete evacuation. In patients with spastic bowel or colon spasms symptoms, the colon remains overactive or hypersensitive even after stool has passed. This continued contraction or tension leads to a lingering sensation of discomfort. Factors like low fiber intake, improper pelvic floor coordination, or underlying anxiety can exacerbate this post-defecation pain. Additionally, inflammation of the nerves in the rectum or colon lining can contribute to heightened pain perception.
3. What causes stomach cramps before pooping?
Stomach cramps before pooping are typically a response to the colon preparing for a bowel movement. In people with spastic colon syndrome, these contractions are more intense and painful due to heightened nerve sensitivity. The gut may misinterpret normal pre-motility signals as threats, resulting in pain or cramping. Psychological stress, hormonal fluctuations (especially in women), and certain food intolerances can increase the likelihood of experiencing such cramps. These symptoms may also be worsened by gastrointestinal dysbiosis or abnormal serotonin signaling in the gut.
4. Can stress really cause colon spasms?
Yes, stress is a well-documented trigger for colon spasm and spastic colon flare-ups. The gut and brain are intricately connected through the vagus nerve and the enteric nervous system. When you’re stressed, cortisol and adrenaline levels spike, which can disrupt gut motility, increase intestinal sensitivity, and promote spasms. Chronic stress can even remodel nerve pathways, making the colon more prone to overreacting. For those with spastic bowel or irritable bowel syndrome and nausea, managing stress through therapy, meditation, or medication can significantly reduce symptoms.
5. What foods should I avoid if I have a spastic colon?
Individuals with a spastic colon should avoid high-FODMAP foods, which ferment in the colon and cause gas, bloating, and cramps. These include onions, garlic, beans, certain fruits, dairy, and artificial sweeteners. Fatty foods, caffeine, and alcohol may also trigger symptoms. Tailoring your diet with the help of a dietitian who understands gastrointestinal disorders is essential. Keeping a symptom diary can help identify specific food triggers contributing to colon pain, bowel movement discomfort, or stomach cramps while pooping.
6. Are colon spasms dangerous?
Colon spasms are not inherently dangerous, but they can cause significant discomfort and affect quality of life. While they do not lead to structural damage, the constant cramping, ache in colon, and unpredictable bowel habits can interfere with daily routines. Persistent symptoms should not be ignored, as they may mimic or mask more serious conditions. Proper evaluation is essential to rule out organic diseases like diverticulitis or colorectal cancer, especially if new symptoms arise suddenly or worsen over time.
7. How do I know if I have IBS vomiting or another issue?
IBS vomiting, though less common than nausea, can occur during severe flare-ups of spastic colon. It is typically functional and not associated with infection or structural disease. If vomiting is frequent, accompanied by weight loss, blood, or occurs at night, further evaluation is needed. Diagnostic workups may include endoscopy, abdominal imaging, and gastric emptying studies to rule out other conditions like gastroparesis or peptic ulcer. Always consult a gastroenterologist to determine the exact cause of vomiting.
8. What causes gastrointestinal spasms apart from spastic colon?
Gastrointestinal spasms can also result from food intolerances, infections, inflammatory diseases, or neurogenic conditions. For instance, lactose intolerance can trigger intense cramps and diarrhea. Bacterial infections like Salmonella or C. difficile may cause spasm due to inflammation and toxin release. Neurological conditions affecting the vagus nerve or autonomic nervous system may also result in abnormal motility. In such cases, symptoms may extend beyond colon pain to include nausea, vomiting, or systemic signs.
9. Can probiotics help with colon cramps?
Probiotics may be beneficial for some individuals with spastic colon or IBS. They can help restore balance to the gut microbiome, reduce inflammation, and improve bowel regularity. Strains like Bifidobacterium infantis and Lactobacillus plantarum have shown promise in reducing colon cramps and irritable bowel nausea. However, probiotic response is highly individual. It’s important to use clinically studied strains and monitor symptom changes. Probiotics are best used as part of a broader treatment plan that includes dietary changes, stress reduction, and possible medication.
10. Is there a cure for spastic colon?
There is currently no cure for spastic colon, but symptoms can be effectively managed with the right approach. Lifestyle modifications, targeted dietary plans (such as low-FODMAP), psychological therapies, medications to regulate motility, and microbiome interventions all play a role. The goal of treatment is not just symptom suppression but long-term remission and quality of life improvement. Ongoing research continues to explore promising treatments, including neuropeptide modulation, microbiota transplants, and gut-brain retraining techniques.

Conclusion
Spastic colon is a multifaceted disorder that goes far beyond occasional discomfort. For millions of people, the daily struggle with colon pain, bowel movement discomfort, and gastrointestinal spasms can feel overwhelming. Yet with scientific understanding, targeted treatment, and compassionate care, relief is not just possible—it’s attainable.
From colon cramps to IBS vomiting and abdominal pain during bowel movements, the symptoms can be daunting. But recognizing that these issues often stem from a combination of neurological sensitivity, dietary triggers, and psychological stress helps reshape how we view and treat this condition. It’s not just about suppressing symptoms—it’s about holistic restoration of gut health, emotional balance, and physical function.
By embracing dietary tools, stress management, and modern medicine, individuals can regain control over their symptoms and live more freely. Continued research into gut-brain interactions, microbiome therapy, and personalized interventions offers even more promise for the future. Whether you’re asking, “Why does my colon hurt?” or “How can I prevent stomach cramps before pooping?”—the answers lie in science, patience, and a proactive approach to healing.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Understanding irritable bowel syndrome and how to manage it
Irritable bowel syndrome: Learn More – Irritable bowel syndrome: What helps – and what doesn’t



