Introduction
As we explore the devastating impacts of dementia, the conversation often centers around memory loss, confusion, and behavioral changes. But what if the disease also alters something as intimate and visible as your facial expression? Does dementia change your face? Could there be subtle facial signs of dementia that precede or accompany cognitive decline? And perhaps most poignantly, is there such a thing as a dementia smile—a seemingly joyful or vacant expression masking a more complex inner state? These questions are gaining attention in both scientific circles and caregiving communities. As the face often serves as a window to the mind, changes in facial expressiveness could be more than a cosmetic shift—they might be a biomarker of neurological health. Understanding the relationship between dementia and facial expressions could help families, clinicians, and caregivers recognize important nonverbal cues, respond more empathetically, and contribute to more timely diagnoses.
You may also like: How to Stop Cognitive Decline: Science-Backed Steps for Prevention and Brain Longevity
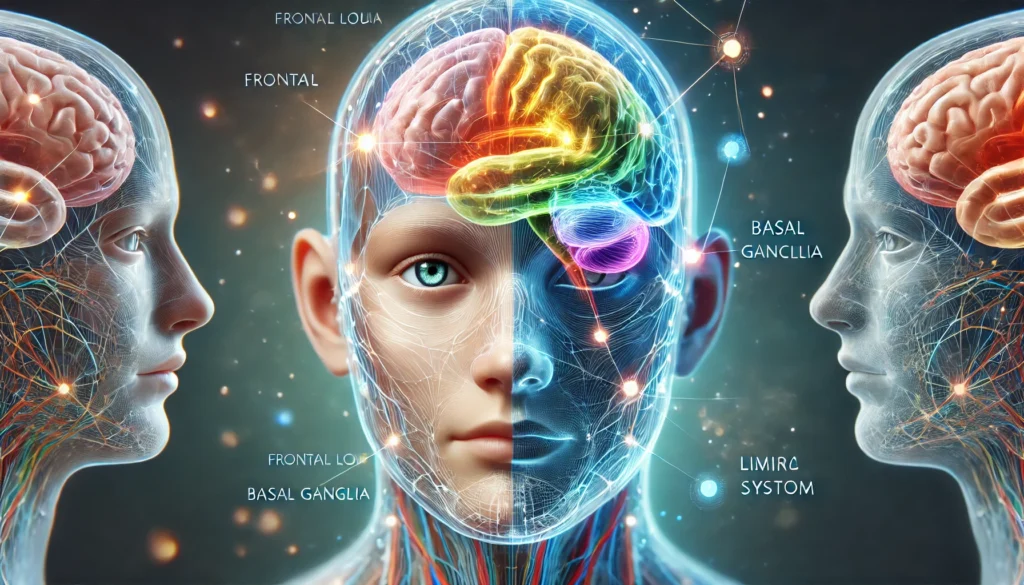
The Neurological Link Between Dementia and Facial Expression
Neurologically, facial expressions are orchestrated by a sophisticated network of brain regions, including the frontal lobe, limbic system, basal ganglia, and brainstem. These regions govern not only our ability to move facial muscles but also our capacity to experience and convey emotion. As dementia progresses, these brain areas often become compromised, leading to diminished facial expressivity, inappropriate expressions, or delayed emotional reactions.
One of the most intriguing phenomena in this context is the so-called dementia smile. Unlike a spontaneous or socially triggered smile, the dementia smile often appears out of context. It may linger for an unusually long time or surface in response to distressing stimuli. While some families find comfort in these moments of perceived joy, others feel confusion or unease, wondering whether the smile reflects genuine emotion or a neurological misfire. In clinical settings, these smiles can be challenging to interpret. They may signal disinhibition, reduced emotional regulation, or even a coping mechanism employed unconsciously by the patient.
In advanced dementia, especially Alzheimer’s disease and frontotemporal dementia, patients may exhibit hypomimia—a condition characterized by reduced facial movement. The face may appear mask-like, with less frequent blinking, diminished eyebrow raises, and fewer smile-related muscle contractions. These facial signs of dementia are not merely aesthetic changes; they represent a deeper decline in neural functioning and emotional responsiveness.

Does Dementia Change Your Face Structurally or Just Expressively?
The question of whether dementia alters the structure of the face or merely its expression is a nuanced one. Structurally, dementia does not reshape bone or alter skin the way some degenerative diseases might. However, chronic disuse of facial muscles, weight loss, dehydration, and a general decline in physical health can make the face appear sunken, tired, or prematurely aged. In this sense, the answer to does dementia change your face is both yes and no.
While the bone structure remains the same, muscle tone and skin elasticity often deteriorate due to nutritional deficiencies, loss of motor coordination, and the general physical regression that accompanies advanced dementia. Additionally, emotional flatness or inappropriate affect—the external display of emotion—can create the perception that the face itself has changed. Caregivers may describe their loved one’s face as “not the same,” referencing not a physical transformation but a loss of familiar expressions, eye contact, and emotional presence.
Some researchers are beginning to investigate facial recognition algorithms and machine learning tools that can detect micro-expressions and subtle facial shifts as potential early indicators of cognitive decline. These technologies aim to quantify the changes that clinicians and families have long observed qualitatively. The field remains young but promising, and it supports the idea that the face could be a critical frontier in early dementia detection.
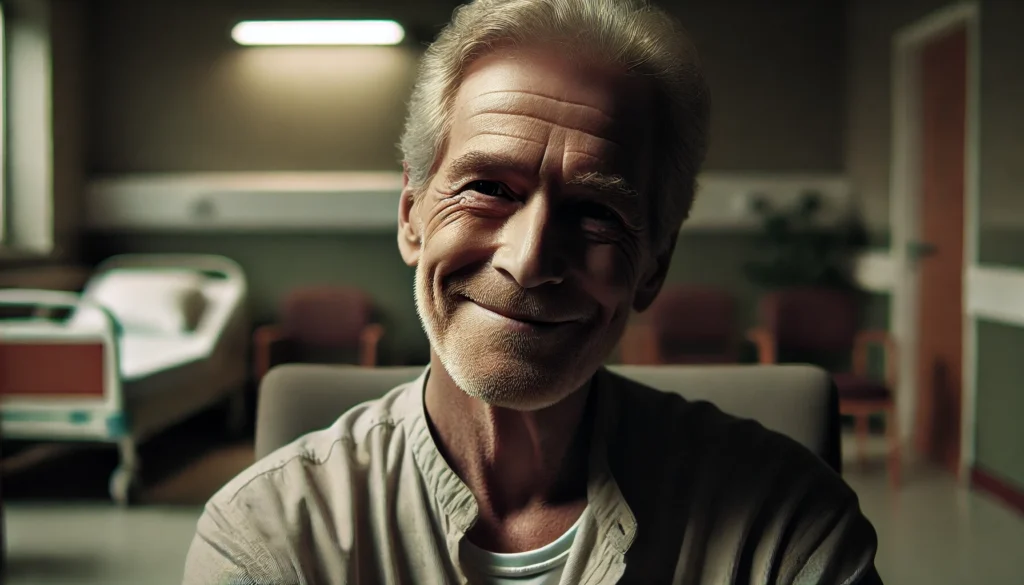
The Dementia Smile: Misunderstood or Meaningful?
Of all the facial signs of dementia, the dementia smile is perhaps the most misunderstood. It can appear endearing, eerie, or simply puzzling, depending on the context. In some cases, the smile may be an automatic social response, deeply embedded in procedural memory. Even as declarative memory fades, the muscle memory of smiling in response to another person may linger. In other instances, the smile might be a result of neurological disinhibition, where the brain fails to suppress inappropriate facial reactions.
Some caregivers report that the dementia smile appears during moments of anxiety, confusion, or pain, suggesting it may serve as a self-soothing behavior. Others observe it during seemingly content interactions, leading to the hopeful interpretation that moments of joy are still accessible to the person. Regardless of its cause, the dementia smile reminds us that emotional experience and expression are not always congruent in people with cognitive impairment.
This discrepancy presents both challenges and opportunities. On one hand, it complicates caregiving and medical assessment. On the other, it opens a window into the resilience of emotional memory and the human capacity for connection even in the midst of neurological degeneration.
Recognizing Facial Signs of Dementia in Everyday Interactions
As the disease advances, people with dementia may show fewer expressions of surprise, concern, amusement, or recognition. The face may lose its ability to reflect inner emotional states, making communication more difficult and caregiving more complex. Understanding these facial signs of dementia can help family members and caregivers adjust their expectations and adapt their approach.
For instance, if a loved one stops responding with smiles, nods, or eyebrow raises, it might be tempting to assume disinterest or emotional detachment. In reality, these shifts may stem from an inability rather than unwillingness to express themselves. Similarly, sudden or inappropriate expressions—such as laughing in sad situations or grinning during an argument—may reflect a breakdown in emotional regulation rather than a lack of empathy.
The way the eyes interact with the environment can also change. Diminished eye contact, delayed blinking, or a glassy stare may signal cognitive decline. These changes often occur subtly at first, reinforcing the need for attentive observation. In some cases, caregivers may be the first to notice that something seems “off” about a person’s facial responses long before more overt memory issues arise.
Cultural Interpretations of Facial Changes in Dementia
Facial expressions and their interpretations are deeply influenced by cultural norms. In some cultures, a smile is expected even in times of distress, while in others, emotional restraint is valued. These cultural factors can influence how the dementia smile and other facial signs of dementia are perceived and responded to.
For example, in East Asian cultures, subtlety and harmony are often emphasized in facial expressions. A lack of overt emotion may be viewed as normal, making the early facial signs of dementia harder to spot. Conversely, in Western cultures where expressiveness is more encouraged, diminished facial animation may be noticed and flagged more quickly.
Understanding these cultural dimensions is essential for clinicians and caregivers working with diverse populations. What might be interpreted as flat affect in one cultural context could be seen as respectful or normal in another. This underscores the importance of knowing the baseline personality and expressive habits of the individual before making assumptions about emotional or cognitive status.
The Role of Facial Expressions in Caregiver Communication
For caregivers, recognizing and interpreting the facial signs of dementia can greatly enhance communication and emotional connection. While verbal communication may become limited, the face often remains a primary tool for interaction. Even in advanced stages, some individuals retain the ability to respond to smiles, laughter, and gentle facial cues.
Caregivers are encouraged to maintain expressive and reassuring facial expressions during interactions. Smiling, nodding, and maintaining eye contact can foster a sense of trust and emotional safety. These gestures may help stimulate emotional memory and provide comfort, even if the individual cannot articulate their feelings.
However, caregivers should also be aware of their own expressions. Frustration, impatience, or sadness can be inadvertently transmitted through facial cues, affecting the mood of the person with dementia. Training programs that include nonverbal communication techniques have been shown to reduce caregiver stress and improve outcomes for patients.
Clinical Relevance of Facial Observation in Diagnosis and Care
While facial expressions alone cannot diagnose dementia, they are increasingly being recognized as valuable observational tools. In clinical assessments, neurologists and psychiatrists often look for signs of reduced expressivity, inappropriate affect, and nonverbal communication deficits. These observations can support a broader diagnostic process that includes cognitive testing, brain imaging, and patient history.
Advanced facial coding systems and emotion recognition software are being developed to assist clinicians in objectively assessing facial changes. These tools analyze micro-expressions—fleeting, involuntary facial movements that can reveal underlying emotional states. By capturing and quantifying these signals, researchers hope to identify early biomarkers of dementia.
Additionally, ongoing monitoring of facial expressiveness can help evaluate disease progression and treatment effectiveness. For example, some medications used to manage dementia symptoms may restore a degree of emotional responsiveness, reflected in improved facial animation. Conversely, increased flatness or inappropriate affect may signal disease advancement or medication side effects.

Social and Psychological Impact of Facial Changes in Dementia
The social ramifications of facial changes in dementia are profound. As facial expressiveness diminishes, social interactions can become strained. Friends may misinterpret flat affect as aloofness, while family members might grieve the perceived “loss” of a loved one’s personality. The face, after all, is a key component of identity.
Patients may also experience psychological distress as they lose control over facial expressions. In the early stages, they may notice that their smile feels forced or that people respond to them differently. This can lead to social withdrawal, depression, and reduced self-esteem. Support groups and counseling can help address these emotional challenges, reinforcing the need for holistic dementia care.
In advanced stages, when insight is lost, the social impact shifts to caregivers. They must navigate a landscape where facial feedback is minimal or misleading, making emotional validation more difficult. This dynamic requires patience, emotional intelligence, and a willingness to accept new forms of connection that may be less reciprocal but no less meaningful.
Frequently Asked Questions
1. What is a dementia smile, and is it a real clinical symptom?
A dementia smile refers to a spontaneous or out-of-context smile that may occur in individuals with cognitive decline. While it is not a formal diagnostic criterion, it is widely observed by caregivers and clinicians. It can reflect disinhibition, preserved muscle memory, or emotional confusion. Though often benign, it may complicate communication and emotional interpretation.
2. Does dementia change your face physically or just the way you express emotion?
Dementia typically does not alter bone structure, but it can affect facial appearance through muscle atrophy, loss of skin tone, and reduced emotional expressiveness. These changes can give the impression that the face itself has changed, even if structurally it has not. Expressive shifts are usually more noticeable than physical ones.
3. What are some early facial signs of dementia?
Early facial signs of dementia may include reduced blinking, less frequent smiling, delayed reactions, and diminished responsiveness in conversation. People may also show fewer micro-expressions or inappropriate emotional responses. These subtle cues can precede more overt cognitive symptoms and may serve as early red flags.
4. How can caregivers interpret changes in facial expression in dementia patients?
Caregivers should consider baseline personality and expressive habits when interpreting changes. A previously expressive person who becomes flat or unresponsive may be exhibiting signs of progression. Conversely, unusual smiles or laughter might indicate confusion, not happiness. Understanding context and maintaining open communication are key.
5. Are there any tools or technologies that detect facial changes related to dementia?
Yes, researchers are developing facial recognition software and emotion detection algorithms to identify micro-expressions and facial anomalies associated with dementia. These tools aim to support early diagnosis and track disease progression. They are still in experimental stages but show promising applications in clinical settings.
6. Can a person with dementia still respond to smiles and facial expressions?
Yes, many individuals with dementia retain the ability to recognize and respond to smiles, especially in early and moderate stages. Nonverbal cues like eye contact, touch, and facial expressions can remain meaningful even as verbal skills decline. These interactions can enhance emotional well-being and foster connection.
7. How do cultural norms affect the recognition of facial signs of dementia?
Cultural expectations around expressiveness can influence how facial changes are perceived. In expressive cultures, reduced animation may be noticed quickly. In more reserved cultures, it may be overlooked or misinterpreted. Clinicians and caregivers should be culturally sensitive and aware of the individual’s normative behavior.
8. Why do some dementia patients appear to smile during distressing moments?
This phenomenon may result from neurological disinhibition, where the brain misfires emotional responses. It can also reflect a coping mechanism or muscle memory unrelated to current emotion. These smiles can be confusing but are not necessarily indicative of happiness or contentment.
9. How can facial signs help track the progression of dementia?
Changes in facial expressiveness can signal shifts in brain function. Increased flatness, inappropriate affect, or total lack of response may indicate disease advancement. Conversely, improved expression after treatment may suggest therapeutic benefit. Monitoring these signs can aid in adjusting care strategies.
10. What can caregivers do to maintain facial expressiveness in loved ones with dementia?
Engaging in activities that stimulate emotion, such as music therapy, reminiscing, or light physical exercise, can help preserve facial responsiveness. Caregivers should also use expressive facial cues themselves to encourage reciprocal interaction. Consistent routines and positive reinforcement can support emotional engagement.

Conclusion
The question of whether dementia changes your face goes far beyond mere appearance. It delves into the essence of human connection, the subtlety of emotional expression, and the profound impact of neurodegenerative disease on identity. From the perplexing nature of the dementia smile to the more clinically observable facial signs of dementia, these nonverbal cues are vital to understanding and supporting those living with cognitive decline.
Facial expressions are not just aesthetic; they are communicative, relational, and diagnostic. They offer insight into the emotional world of someone who may no longer have the words to express it. As research continues to explore how dementia affects the face, the goal remains clear: to provide compassionate, personalized, and scientifically grounded care. By recognizing and respecting the facial signs of dementia, we open the door to deeper empathy, more accurate assessments, and a fuller appreciation of the human experience within dementia’s grasp.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Early Diagnosis of Dementia and Alzheimer’s: Why Timely Detection Matters for Better Brain Health
Does My Mother Have Dementia? How to Recognize Early Signs and What to Do Next



