Introduction
As the global population continues to age, the prevalence of neurodegenerative diseases such as Alzheimer’s and related dementias is rapidly increasing. These conditions not only place significant emotional and financial burdens on individuals and families but also present growing challenges for healthcare systems worldwide. Despite decades of research, there is still no definitive cure for dementia. However, there is an area where major strides can be made: early identification. The early diagnosis of dementia, including Alzheimer’s disease, is critical for optimizing patient outcomes, managing symptoms effectively, and providing families with the tools they need to navigate the road ahead. Timely detection gives people the opportunity to access interventions that could delay the progression of symptoms, plan for the future with clarity, and make informed lifestyle and care decisions.
You may also like: How to Stop Cognitive Decline: Science-Backed Steps for Prevention and Brain Longevity
There has been a growing movement among scientists, clinicians, and public health experts advocating for alzheimer early detection strategies, from improved screening tools to increased awareness of early warning signs. By recognizing subtle changes in cognition and behavior before they evolve into more debilitating symptoms, early intervention becomes possible. Through a blend of scientific advancements and increased community education, early detection has the potential to transform the dementia care paradigm and enhance quality of life for millions.
Understanding Dementia and Alzheimer’s Disease
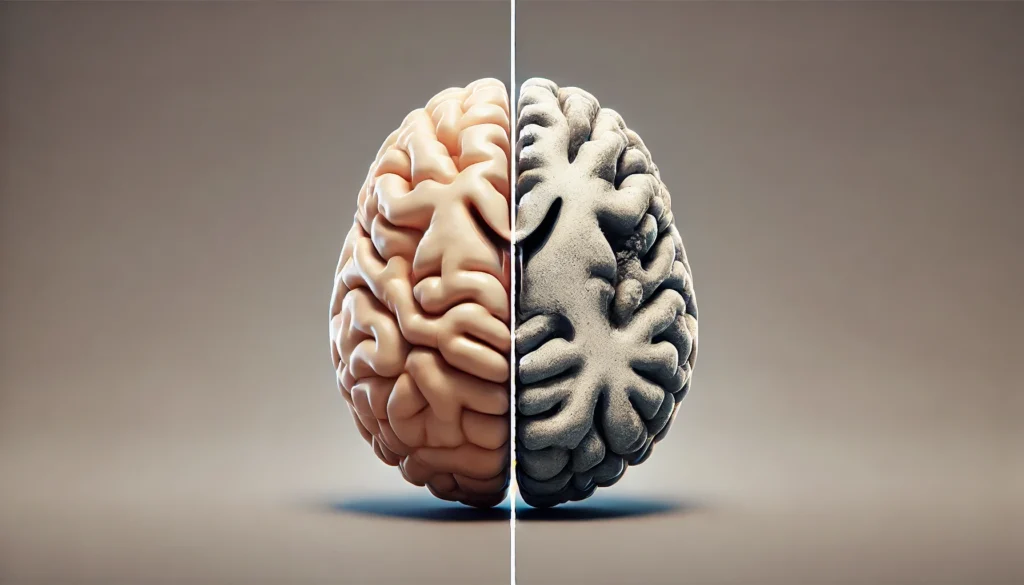
Dementia is an umbrella term that encompasses a range of cognitive disorders characterized by memory impairment, behavioral changes, and a decline in thinking and reasoning skills. Alzheimer’s disease is the most common cause of dementia, accounting for an estimated 60 to 80 percent of all dementia cases. The condition is progressive and involves the accumulation of abnormal protein deposits in the brain, leading to the degeneration and death of brain cells.
The symptoms of dementia can vary widely, depending on the underlying pathology and areas of the brain affected. Common symptoms include memory loss, difficulty with language, impaired judgment, and mood or personality changes. While age is the greatest known risk factor, dementia is not a normal part of aging. In fact, one of the central arguments for the early diagnosis of dementia is that too often, symptoms are dismissed as “just getting older,” delaying appropriate medical evaluation.
Alzheimer early detection efforts are focused on identifying changes in the brain and cognitive function long before symptoms become severe. This involves recognizing the early stages of mild cognitive impairment (MCI), particularly the subtype known as amnestic MCI, which can precede Alzheimer’s disease. People with MCI may have subtle but noticeable changes in memory or thinking that are measurable but not severe enough to interfere with daily activities. Not everyone with MCI progresses to dementia, but a significant percentage do, especially when underlying Alzheimer’s pathology is present.
Why Early Diagnosis Matters
One of the strongest arguments for the early diagnosis of dementia is the opportunity it provides for medical and personal planning. When dementia is diagnosed early, individuals have a greater capacity to understand and participate in discussions about their care preferences, financial planning, and legal arrangements. This can include setting up powers of attorney, creating advanced directives, and deciding on living arrangements while the individual still has the cognitive ability to make informed decisions.
From a medical standpoint, early detection opens the door to treatments that may help manage symptoms and slow disease progression. While current medications do not cure Alzheimer’s, they can offer symptom relief and preserve function for a longer period when started early. New disease-modifying therapies are also being developed, and early detection is crucial for identifying candidates who may benefit from clinical trials and emerging interventions.
Additionally, alzheimer early detection provides the opportunity for individuals to adopt lifestyle changes that have been associated with reduced cognitive decline. These include regular physical activity, cognitive training, heart-healthy diets such as the Mediterranean diet, improved sleep habits, and better management of conditions like hypertension, diabetes, and depression. When patients and families understand the nature of the disease early on, they are more likely to engage in these beneficial activities.
Emotionally, early diagnosis can reduce uncertainty and empower individuals and their caregivers. Rather than wondering what might be wrong, patients can gain clarity and begin to seek support. Caregivers also benefit from having time to prepare, access resources, and build support networks.
Recognizing Early Signs and Symptoms
To achieve effective early diagnosis of dementia, public and professional awareness of early signs must be prioritized. The initial symptoms of Alzheimer’s disease and other dementias can be subtle and gradual, making them easy to overlook. However, when these signs are identified early and contextualized within a broader medical evaluation, they can lead to earlier and more accurate diagnoses.
Early warning signs may include forgetting recently learned information, misplacing objects and being unable to retrace steps, confusion with time or place, difficulty completing familiar tasks, trouble finding the right words, and changes in mood, personality, or social engagement. It is especially important to differentiate between normal age-related memory changes and the more serious memory lapses associated with early cognitive impairment.
Primary care physicians are often the first point of contact for patients with cognitive complaints. Therefore, it is essential that they are trained to recognize these early indicators and refer patients for further cognitive assessment when warranted. A proactive and attentive approach in primary care can significantly improve rates of alzheimer early detection and connect patients with neurologists, geriatricians, and neuropsychologists for comprehensive evaluation.

Tools and Technologies for Early Detection
The evolution of diagnostic technologies has significantly enhanced the potential for early diagnosis of dementia. A combination of cognitive assessments, imaging techniques, and biomarker analyses are increasingly being used to identify Alzheimer’s and other dementias at earlier stages.
Neuropsychological testing remains a cornerstone of early diagnosis. These tests evaluate various cognitive domains, such as memory, attention, language, executive function, and visuospatial skills. Patterns of deficits can help distinguish between different types of dementia and identify MCI.
Neuroimaging methods such as magnetic resonance imaging (MRI) and positron emission tomography (PET) scans can reveal structural and functional changes in the brain. For example, PET scans can detect beta-amyloid plaques, a hallmark of Alzheimer’s pathology, years before symptoms appear. MRI can identify atrophy in key brain areas such as the hippocampus, which is affected early in Alzheimer’s disease.
Advances in blood-based biomarkers are revolutionizing the field. New tests are being developed that can measure levels of amyloid, tau proteins, and neurofilament light chain (NfL) in the blood. These biomarkers have the potential to offer non-invasive, cost-effective screening tools for alzheimer early detection, especially in primary care settings.
Genetic testing may also play a role in early detection, particularly for individuals with a family history of Alzheimer’s disease. While not everyone with genetic risk factors will develop dementia, understanding one’s genetic predisposition can prompt earlier monitoring and intervention.

Barriers to Early Diagnosis
Despite the clear benefits, multiple barriers still hinder the early diagnosis of dementia. One major issue is stigma. Many individuals are reluctant to seek help for memory problems due to fear, denial, or misconceptions about aging. Cultural attitudes may also influence how symptoms are perceived and whether medical evaluation is pursued.
Another challenge lies in the variability of symptoms and the overlap with other conditions. Depression, medication side effects, sleep disorders, and even vitamin deficiencies can mimic early dementia symptoms, leading to misdiagnosis or missed diagnoses.
Healthcare provider limitations are also a factor. In busy clinical settings, there may be limited time to conduct in-depth cognitive assessments or discuss cognitive concerns thoroughly. Additionally, some providers may lack training in dementia recognition or feel uncomfortable delivering such diagnoses.
Systemic barriers such as lack of access to specialists, especially in rural or underserved areas, contribute to diagnostic delays. Insurance coverage and cost considerations can also prevent patients from accessing advanced diagnostic tools or specialist consultations.
To overcome these barriers, healthcare systems need to invest in clinician training, increase access to diagnostic services, reduce stigma through public education, and incorporate cognitive health into routine wellness checks.
The Role of Caregivers and Families
Families and caregivers play a pivotal role in the early diagnosis of dementia. They are often the first to notice changes in a loved one’s memory, behavior, or functioning. Encouraging open dialogue and bringing concerns to a medical provider’s attention can be the first step in the diagnostic journey.
Caregivers also serve as valuable sources of collateral information during the diagnostic process. Because individuals with early cognitive impairment may lack insight into their deficits, the observations of close family members become essential in providing context to clinicians. This collaboration leads to a more accurate assessment and a better understanding of how symptoms affect day-to-day life.
Families should be educated about the importance of early detection and be empowered to advocate for comprehensive cognitive evaluations when necessary. Resources such as caregiver support groups, educational seminars, and dementia advocacy organizations can help caregivers recognize symptoms, access appropriate care, and feel supported in their roles.
Innovations in Screening and Community Outreach
As the demand for early diagnosis of dementia grows, innovative screening programs are being developed to reach more individuals at earlier stages. These include digital tools, telemedicine platforms, and community-based initiatives aimed at improving access to cognitive assessment.
Online cognitive testing platforms and smartphone-based apps are increasingly used for initial screening. These tools can assess memory, attention, and reaction time, providing users with feedback and encouraging them to seek further evaluation when warranted. While not a substitute for formal diagnosis, digital screening tools can serve as a gateway to medical consultation.
Telehealth has emerged as a powerful tool for early detection, especially in areas with limited access to specialists. Virtual cognitive assessments conducted by neurologists or neuropsychologists can bridge geographical gaps and connect patients to expert care from the comfort of their homes.
Community-based programs that offer free memory screenings, dementia education workshops, and caregiver support are also instrumental in raising awareness and facilitating early diagnosis. Partnerships with libraries, senior centers, and faith-based organizations help bring cognitive health resources to the local level.
Prevention and Risk Reduction Strategies
Although dementia cannot always be prevented, growing evidence supports the idea that modifying certain lifestyle factors can reduce risk or delay onset. The World Health Organization and other major public health bodies now promote dementia risk reduction as a central strategy.
Physical activity, particularly aerobic exercise, has been shown to enhance brain health and reduce dementia risk. Regular exercise improves cerebral blood flow, reduces inflammation, and stimulates the release of brain-derived neurotrophic factor (BDNF), which supports neuron growth and survival.
Nutrition also plays a crucial role. Diets rich in whole grains, fruits, vegetables, fish, and healthy fats—such as the Mediterranean or MIND diet—have been associated with better cognitive outcomes. Limiting processed foods, saturated fats, and excessive sugar can also support brain health.
Cognitive engagement and social interaction help build cognitive reserve. Lifelong learning, hobbies, volunteerism, and maintaining strong social networks contribute to mental resilience. Similarly, addressing hearing loss, managing stress, and ensuring quality sleep are increasingly recognized as important components of dementia prevention.
Early diagnosis of dementia allows individuals to implement these changes while cognitive function is still relatively intact, potentially altering the course of the disease.
The Future of Early Detection
The future of dementia care will be shaped by continued advancements in early detection. Artificial intelligence (AI) and machine learning are already being integrated into cognitive assessments, helping identify patterns and subtle deficits that might elude traditional methods. AI-driven tools could make screenings more accessible, faster, and more accurate.
Researchers are also exploring novel biomarkers and imaging techniques that could further refine alzheimer early detection. These may include retinal imaging to detect amyloid deposits in the eye, or advanced blood panels that identify neurodegenerative markers with high sensitivity and specificity.
Personalized medicine is another promising frontier. As our understanding of genetic risk factors and individual disease trajectories deepens, tailored prevention and intervention strategies will become possible. Genetic counseling, precision nutrition, and customized cognitive training are likely to play greater roles in future care models.
Policy and healthcare reform will also be essential. Integrating cognitive health into routine primary care visits, providing reimbursement for early diagnostic services, and supporting research initiatives will ensure that the benefits of early detection reach all communities.
Ultimately, early diagnosis of dementia has the potential to shift the narrative from crisis management to proactive, empowered care. With continued investment, innovation, and awareness, early detection can become the standard rather than the exception.
Frequently Asked Questions
1. What is the earliest age at which dementia symptoms can appear?
While dementia is more common in individuals over the age of 65, early-onset dementia can occur in people as young as their 30s or 40s. Alzheimer early detection in younger individuals is crucial, as symptoms are often misattributed to stress or other conditions. Early diagnosis allows for timely interventions and lifestyle adjustments that may slow disease progression.
2. How does early diagnosis of dementia impact long-term care planning?
Early diagnosis gives individuals and their families the chance to make informed decisions about long-term care, legal matters, and financial planning. With time on their side, patients can participate actively in these discussions and choose care preferences, appoint decision-makers, and organize resources in a thoughtful and proactive way.
3. Are there specific tests available for alzheimer early detection?
Yes, a variety of tests are now available for early detection of Alzheimer’s. These include cognitive assessments, MRI and PET scans, and emerging blood-based biomarkers that detect amyloid and tau proteins. Combining multiple tests enhances diagnostic accuracy, especially when interpreted by a specialist.
4. Can early diagnosis prevent the progression of dementia?
While early diagnosis cannot stop dementia, it can slow its progression through medications, lifestyle changes, and supportive therapies. Identifying the condition early allows for interventions that may preserve cognitive function and delay the onset of more severe symptoms.
5. What are the barriers preventing people from seeking early diagnosis?
Common barriers include stigma, fear of the diagnosis, lack of awareness, and limited access to specialists. In some cases, healthcare providers may not recognize early symptoms or may attribute them to normal aging. Overcoming these barriers requires public education and system-level changes in healthcare.
6. How accurate are current screening tools for early-stage dementia?
While no single test is perfectly accurate, current screening tools are increasingly reliable when used in combination. Neuropsychological assessments, imaging, and biomarker tests provide a comprehensive picture. Ongoing research is continually improving the precision and accessibility of these tools.
7. Should everyone get screened for dementia after a certain age?
Routine cognitive screening is not yet standard for all adults, but individuals with memory concerns, family history of dementia, or other risk factors may benefit from early evaluation. Many health organizations recommend discussing cognitive health during annual checkups, especially for adults over 65.
8. How do caregivers contribute to alzheimer early detection?
Caregivers often notice subtle behavioral changes and memory lapses before others do. Their observations can prompt early medical evaluations and offer critical context during the diagnostic process. Encouraging caregivers to voice their concerns is vital in achieving timely diagnosis.
9. What role does lifestyle play after an early dementia diagnosis?
Lifestyle factors are incredibly important. Exercise, nutrition, cognitive training, stress management, and social engagement can all help preserve cognitive function. Early diagnosis provides a window of opportunity to adopt these habits before significant decline sets in.
10. Can online tests accurately detect early signs of dementia?
Online cognitive tests can provide helpful preliminary information and encourage people to seek further evaluation. However, they are not a substitute for a professional diagnosis. If a test raises concerns, individuals should consult a healthcare provider for a comprehensive assessment.

Conclusion
The early diagnosis of dementia, particularly through alzheimer early detection efforts, is one of the most powerful tools we have in the fight against cognitive decline. By identifying signs and symptoms in their initial stages, individuals gain access to vital treatments, support, and planning resources that can dramatically improve quality of life. Equally important, early diagnosis opens the door to preventive strategies that may delay or mitigate the effects of neurodegenerative diseases.
In today’s evolving medical landscape, the focus is shifting from reaction to prevention, and early detection lies at the heart of this transformation. It empowers patients and caregivers with knowledge, reduces the burden of uncertainty, and fosters more compassionate, personalized care. By investing in education, technology, and access to care, society can embrace a new model of dementia care—one rooted in dignity, foresight, and hope.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.



